|
 |
- Search
| Healthc Inform Res > Volume 21(2); 2015 > Article |
Abstract
Objectives
The widespread adoption of health information technology (IT) will help contain health care costs by decreasing inefficiencies in healthcare delivery. Theoretically, health IT could lower hospitals' malpractice insurance premiums (MIPs) and improve the quality of care by reducing the number and size of malpractice. This study examines the relationship between health IT investment and MIP using California hospital data from 2006 to 2007.
Methods
To examine the effect of hospital IT on malpractice insurance expense, a generalized estimating equation (GEE) was employed.
Results
It was found that health IT investment was not negatively associated with MIP. Health IT was reported to reduce medical error and improve efficiency. Thus, it may reduce malpractice claims from patients, which will reduce malpractice insurance expenses for hospitals. However, health IT adoption could lead to increases in MIPs. For example, we expect increases in MIPs of about 1.2% and 1.5%, respectively, when health IT and labor increase by 10%.
Conclusions
This study examined the effect of health IT investment on MIPs controlling other hospital and market, and volume characteristics. Against our expectation, we found that health IT investment was not negatively associated with MIP. There may be some possible reasons that the real effect of health IT on MIPs was not observed; barriers including communication problems among health ITs, shorter sample period, lower IT investment, and lack of a quality of care measure as a moderating variable.
Health information technology (IT), such as Electronic Health Record (EHR), comprises tools to increase efficiency and to increase communication among providers within and between organizations by the automating the collection, use, and storage of patient information. Health IT has been reported to increase the quality of care by increasing adherence to guidelines; improving the aggregation, analysis, and communication of patient information; supporting diagnostic and therapeutic decision-making; preventing adverse events; and providing alerts and clinical warnings [1,2]. In addition, health IT allows tracking of therapy in detail, so that physicians can address adherence and compliance issues [3]. Thus, health IT can improve efficiency and reduce redundant care by improving continuity in information transfer and communication among healthcare providers.
Thus, the widespread adoption of health IT can help contain healthcare costs by reducing inefficiency and improving quality of care in healthcare delivery. Many single-site studies at academic hospitals have provided evidence that specific functions of the Electronic Medical Record (EMR), including clinical decision support or computerized physician order entry, may improve quality by reducing errors [4,5,6]. Other studies with large samples of hospitals have found evidence that overall spending on health IT is associated with improved patient safety, higher quality of care, and reduced costs [1,7,8,9,10]. Moreover, the Institute of Medicine (IOM) has encouraged adopting EMR to reduce medical errors and healthcare costs, and the American Recovery and Reinvestment Act of 2009 established financial incentives for hospitals to promote the adoption and meaningful use of health IT.
Accordingly, theoretically, health IT could improve quality of care by reducing the number and size of malpractice cases and eventually lower hospitals' malpractice insurance premiums (MIPs). According to the Certification Commission for Healthcare Information Technology (CCHIT), if a hospital can demonstrate to malpractice insurers that it has instituted appropriate technologies and processes, a malpractice insurer assumes the financial risk with the expectation that a hospital's investment in technologies and processes will enable 1) the hospital to avoid mistakes and intercept errors before they harm patients and 2) the insurer to obtain electronic records and seek the cause when an error occur [11]. Also, CCHIT asserted that the adoption of health IT may improve defense against liability claims by improving medical record documentation. If the insurer is better prepared to defend the case through health IT, the results of settlement negotiations and jury trials may be more favorable to them.
Hospitals may receive further discounts in MIPs in the future by providing demonstrable high quality patient care [12]. Actually, some hospitals have had discounted MIPs because of the adoption of EMR [13,14,15]. These studies examined the effect of health IT investment on MIP. It appears that some malpractice insurers think that the use of health IT will decrease malpractice claims. Thus, they offer the discount for policy holders who have adopted health IT.
Thus, a hospital's adoption of health IT and an insurer's premium are influenced by the expected benefits from health IT when determining an MIP. Both of them expect that health IT will monitor, control, and reduce information asymmetry between clinicians and the hospital and between the hospital and the insurer; health IT may reduce MIPs through improving quality of care and reducing medical errors in hospitals. However, to the best of our knowledge, no researchers have examined the impact of health IT on future quality of patient care measured by MIP. Therefore, this study examined the relationship between health IT investment and MIP using California hospital data from 2006 to 2007.
The hospital financial data in the Office of Statewide Health Planning and Development (OSHPD) and annual survey of hospital by American Hospital Association (AHA) data were utilized in this study. The OSHPD's hospital financial data include hospital characteristics, patient utilization, and financial information, including balance sheets, income statements, cash flow, etc. In the OSHPD, individual hospital financial disclosure reports are available beginning with reporting periods ending in 2002, The data are updated continuously, and they include reports as originally submitted by each hospital and as desk audited by the OSHPD. The overall sample size was 483.
These hospital financial data have been used in many healthcare and economic studies [2,16,17]. The AHA data profiles more than 6,500 hospitals throughout the United States. The response rate for the AHA annual survey has been more than 70% each year. The survey is conducted to maximize accuracy and participation (see detailed process in http://www.ahadataviewer.com/about/data/). AHA data are used by government agencies, media, and the industry for accurate and timely analysis and decision-making. This database contains hospital-specific data on hospitals and healthcare systems (except federal government hospitals), including organization location, size, structure, personnel, and hospital. For this study, acute care hospitals observed in two consecutive years were included. Two-hundred acute care hospitals were included for each year from 2006 to 2007, so the final sample size was 400 overall.
The dependent variable was the MIP defined as the cost incurred related to professional liability insurance and the cost of self-insurance that has been actuarially determined. This information could be observed in the 'trial balance worksheet and supplemental expense' of the California hospital financial data.
Three groups of variables were employed: 1) hospital and market characteristics, 2) the volume of hospital service, and 3) health IT. Hospital characteristics included hospital and market characteristics, such as ownership, teaching status, number of beds, network hospital status, competition, and case mix index (CMI). Hospital ownership was measured by two dummy variables, namely, not-for-profit and government, with for-profit hospitals representing the reference. Teaching status was a dummy variable indicating Council of Teaching Hospitals (COTH) membership. Beds were categorized into five specialized types of beds, including general acute beds for adults, pediatrics, obstetrics, cardiac intensive care, and neonatal intensive care. A network hospital was represented by a dummy variable entitled system membership. To measure the competitiveness of a given geographical market based on health service area (HSA), each hospital's share of adjusted admissions were calculated by summing the total admissions and outpatient visits for each hospital [18]. Then, the share of adjusted admissions for each hospital for each HSA was calculated. Lastly, this share of adjusted admission was squared and summed by HSA to obtain market competition or the Herfindahl-Hirschman Index (HHI). The HHI is an economic concept widely used as to measure competition [19,20,21,22]. The CMI is a measure of the relative resources needed to treat the mix of patients in each California hospital during a given calendar year. The OSHPD utilizes Medicare Severity-Diagnosis Related Groups (MS-DRG) to calculate the CMI, and their associated weights, assigned to each MS-DRG by the Centers for Medicare & Medicaid Services (CMS). Then, each record is assigned an MS-DRG accounting for principal and secondary diagnoses, age, procedures performed, the presence of comorbidities and/or complications, discharge status, and gender. Lastly, the OSHPD applies them to all patient discharge data during the course of a calendar year [23]. Volume includes total admissions, outpatient visits, percentage of Medicare and Medicaid admissions out of total admissions, emergency room (ER) visits, and the numbers of inpatient and outpatient surgical operations. Lastly, our key independent variables were health IT investment measured as IT capital as well as IT labor [2,16]. The OSHPD data places all IT expenditures within the data processing section of financial statements. Health IT capital and IT labor were extracted from each hospital's balance sheet. While health IT capital includes physical capital, purchased service, lease and rental and other direct expenditure, IT labor includes salaries and wages, employee benefits, and professional fees.
To examine the effect of health IT on MIPs, a GEE was employed, which is used in many health care studies. The GEE can control variance structure and clustering error within hospitals. For the model selection, we tested quasi-likelihood under the independence model criterion (QIC) and chose the independent variance model with the smallest QIC among many possible variance structures [24]. The regression model is expressed as where MIP represents malpractice insurance premium. HC represents hospital and market characteristic vector including hospital ownership (for-profit, not-for-profit, and government hospitals), teaching status (COTH member), specialized number of beds (general acute beds for adults, pediatrics, obstetrics, cardiac intensive care, and neonatal intensive care), network hospital status, competition measured by HHI, and CMI. Volume represents the patient utilization vector, including total admissions, outpatient visits, percentage of Medicare and Medicaid ER visits, and numbers of inpatient and outpatient surgical operations. IT includes IT capital and IT labor investment. We took a log in MIP and IT investment because log transformations make skewed distribution more normal. Year represents dummies for 2007 years. All analyses were conducted using STATA ver. 11.2 (STATA Corp., College Station, TX, USA).
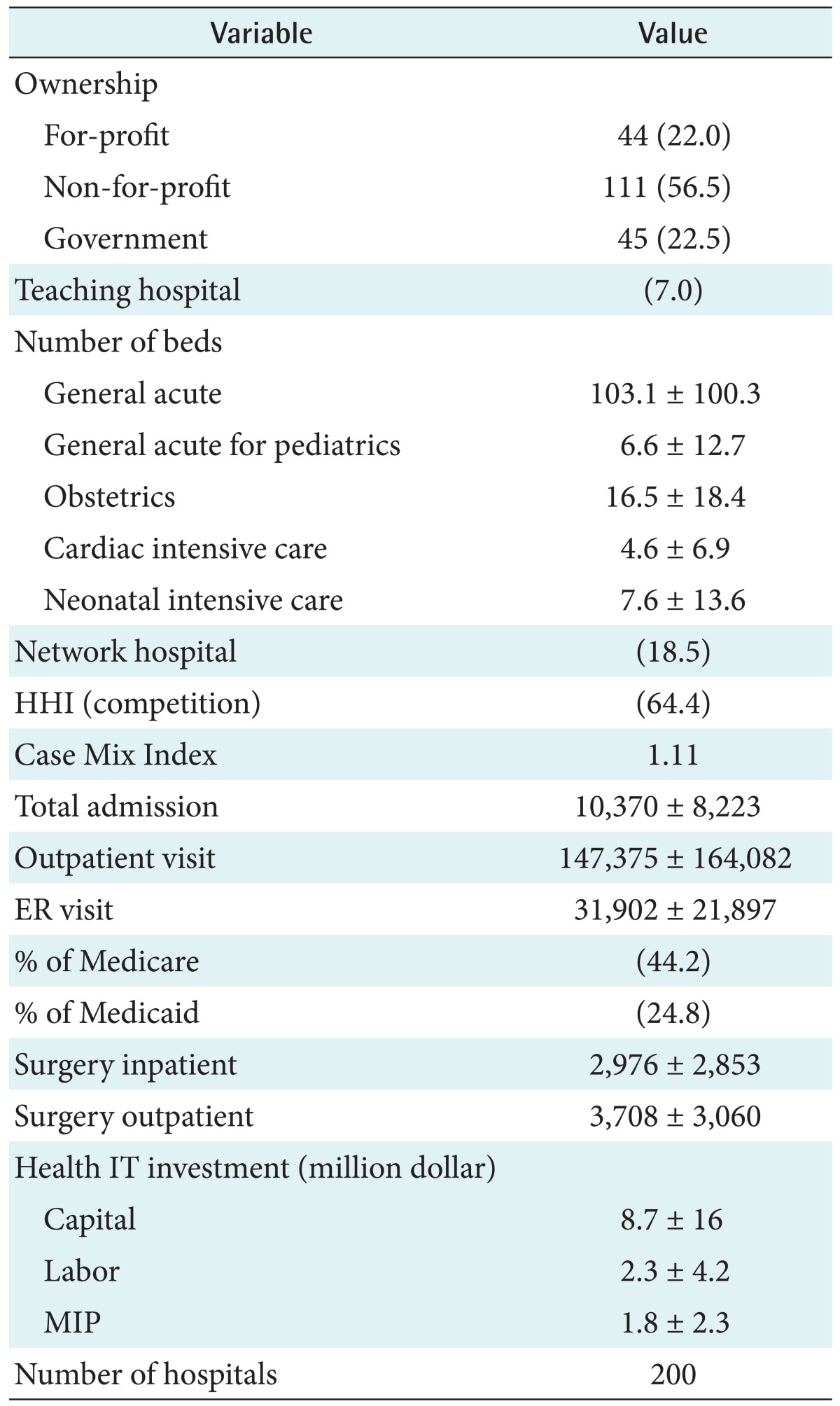
Table 1 shows descriptive statistics. Not-for-profit hospital ownership accounted for 55.3%. Teaching hospitals account for only 7% of the total sample. The numbers of beds varied according to type; the number of general acute care beds was 103, general acute for pediatrics was 6.6, obstetrics 16.5, cardiac intensive care 4.5, and neonatal intensive care 7.6. Network hospitals accounted for 18.5%. Competition measured as HHI was 64.6%, and CMI was just over 1. The volume of outpatient visits was the largest compared to the total admissions and ER visits. The percentages of Medicare and Medicaid admissions were 44.2% and 24.8%, respectively. The number of surgeries during outpatient visits was almost 1.2 times larger than that during inpatient visits. Health IT capital investment was much larger than that of IT labor; $8.7 million for IT capital and $2.3 million for IT labor. Last, MIP was $1.8 million.
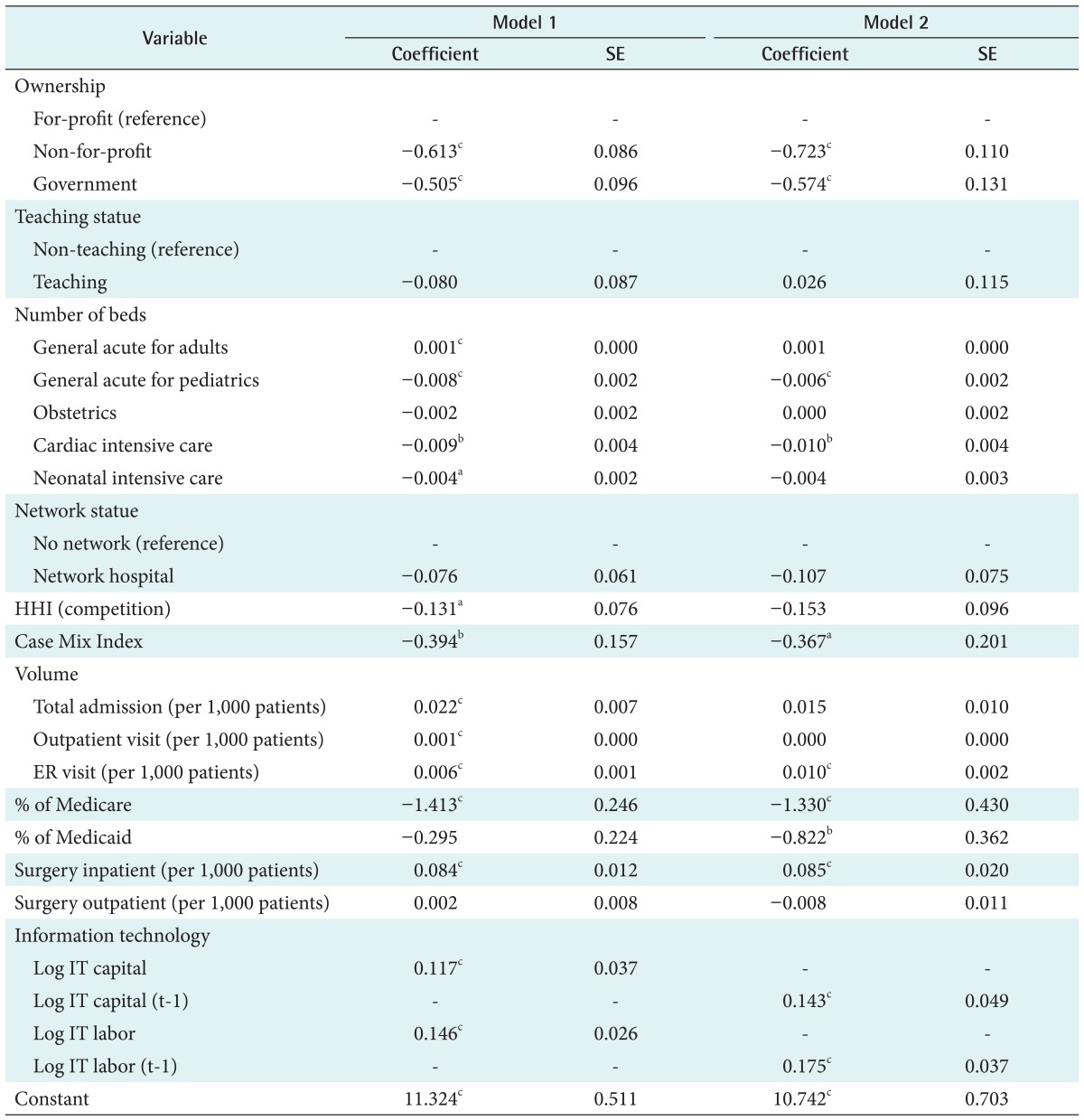
Table 2 shows the GEE regression results. As seen in the table, health IT capital and IT labor investment were positively associated with MIP in model 1. For example, we expect about 1.2% and 1.5% increases in MIP when health IT and labor increase by 10%, respectively. Moreover, we found other significant variables related to MIP. Ownership plays an important role. Not-for-profit and government hospital statuses were negatively associated with MIP. Also, the types of beds are important factors in determining MIP. For example, general acute beds for adults had a small but significant impact on MIP. However, beds for general acute, pediatrics, cardiac intensive care, and neonatal intensive care were negatively associated with MIP. We also found that higher competition and lower CMI led to higher MIP. Hospital volumes including total admissions, outpatient visits, and ER visits, were positively associated with MIP as expected. However, the percentage of Medicare admissions led to lower MIP. Also, the number of surgical inpatient visits was associated with higher MIP.
As shown in the second column (mode 2) of Table 2, we measured the lagged health IT investment on MIP because health IT could be effective by learning by doing [8]. However, we also found that health IT capital and IT labor were positively associated with MIP. Other variables showed similar relationships with MIP as in model 1.
This study examined the effect of health IT investment on MIP controlling other hospital, market, and volume characteristics. It appears that some malpractice insurers think that the use of health IT will decrease malpractice claims. Thus, they offer discounts to policy holders who have adopted health IT systems, such as EMR. For example, policyholders in Texas who documented EMR use for at least one year can have their MIPs discounted by 2.5% [13]. Also, providers that have implemented certified EMR in the Midwest can qualify for credit of between 2% and 5% from their medical insurance company [14]. Blue Cross and Blue Shield of New Jersey offer premium discounts to providers who have implemented approved EMR systems [15].
However, contrary to previous expectations, this study found that health IT investment was positively associated with MIP. There may be four possible explanations. First, there are many barriers of health IT investment [25,26,27]. For example, physicians have workflow disruption; they may not have enough time to become familiar with health IT and train to use it. Also, other barriers were listed as concerns about security and privacy, complexity in the documenting process, and lack of computer skills, among others. In addition, communication may be an important barrier. Health IT systems, including EMR and computerized patient order entry (CPOE), may not communicate with each other, although they are intended to prevent medical errors and improve patient outcomes. Some previous studies also doubted the effect of EMR on the risk of being sued because most EMR charts are template-driven. Also, current EMR systems are not able to communicate with one another. Thus, superfluous or inaccurate information may often creep into a documented patient visit [28]. Also, several lawyers have argued that the default settings of an EMR could present almost no opportunities for physicians to add information to medical records. Also, EMR could provide too much information. For instance, the risk of being sued may increase if an EMR provides too many alerts or warnings that physicians do not respond to. Thus, these kinds of barrier may prevent health IT from being effective.
Second, our sample only covered a short duration of two years, so it may not reflect the real effect of health IT investment on MIP; some studies found that health IT could be effective 3 to 5 years after adoption [2,8,16,18]. Third, lower health IT investment may not be effective in reducing MIP. For example, Victoroff et al. [29] evaluate the effect of EHR use on medical liability claims in a population of office-based physicians, including claims that could potentially be directly prevented by features available in EHRs. They argued that the lack of significant effect may be due to a low prevalence of EHR-sensitive claims. Similarly, in our sample, the health IT capital investment was just around 5% out of total revenue. Compared to other IT industries (around 9%), this ratio is too low. Thus, this lower IT investment may not lead to reduced MIP. Another concern is that health IT investment may lead to a larger number of malpractice suits because patients may have more scientific evidence for them. However, in the current stage of health IT adoption in the years of 2006 and 2007, only a small number of hospitals had adopted EMR systems, and the amount of health IT investment was low in each hospital [2]. Thus, this concern may not apply to the current stage of health IT investment. However, this argument may be applicable for more recent data.
Lastly, the quality of care could be a moderating variable in this analysis. For example, the quality of care may reduce MIP but health IT investment may have a direct effect. Thus, the lack of quality of care measurement in the analysis may have led to biased estimates.
Even though we could not find a negative relationship between health IT and MIP as expected, it was the first study to examine the effect of health IT investment on MIP at a hospital level. Unlike physicians, hospitals' MIPs are based on the experience rating. Thus, if a hospitals' claims experience is more stable over time after more health IT investment, the MIP related to the hospital will be reduced.
In conclusion, we examined the effect of health IT on quality of care measured by MIPs using two years of California hospital data and found that health IT was not negatively associated with MIP. There may be three possible limitations of this study such that the real effect of health IT on MIPs may not have been observed, including communication problems among health ITs, the short sample period, and low IT investment.
The study results imply that the hospital managers and insurers should be cautious to interpret the effect of health IT on MIP and that they should remember that EMR adoption itself may not lead to improved quality of care or reduce MIP. Instead, it could increase MIP by worsening the quality of care without working with IT vendors and physicians at the same time of EMR adoption.
References
1. Parente ST, McCullough JS. Health information technology and patient safety: evidence from panel data. Health Aff (Millwood) 2009;28(2):357-360. PMID: 19275990.


2. Lee J, McCullough JS, Town RJ. The impact of health information technology on hospital productivity. Rand J Econ 2013;44(3):545-568.

3. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academies Press; 2001.

4. Kuperman GJ, Gibson RF. Computer physician order entry: benefits, costs, and issues. Ann Intern Med 2003;139(1):31-39. PMID: 12834316.


5. Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA 2005;293(10):1223-1238. PMID: 15755945.


6. Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144(10):742-752. PMID: 16702590.


7. Parente ST, Van Horn RL. Valuing hospital investment in information technology: does governance make a difference? Health Care Financ Rev 2006;28(2):31-43. PMID: 17427843.



8. Borzekowski R. Measuring the cost impact of hospital information systems: 1987-1994. J Health Econ 2009;28(5):938-949. PMID: 19699542.


9. Yu FB, Menachemi N, Berner ES, Allison JJ, Weissman NW, Houston TK. Full implementation of computerized physician order entry and medication-related quality outcomes: a study of 3364 hospitals. Am J Med Qual 2009;24(4):278-286. PMID: 19502568.



10. Himmelstein DU, Wright A, Woolhandler S. Hospital computing and the costs and quality of care: a national study. Am J Med 2010;123(1):40-46. PMID: 19939343.


11. Certification Commission for Healthcare Information Technology. CCHIT certified electronic health records reduce malpractice risk. [place unknown]: Certification Commission for Healthcare Information Technology; 2007.

12. Sloan FA, Shadle JH. Is there empirical evidence for "Defensive Medicine"? A reassessment. J Health Econ 2009;28(2):481-491. PMID: 19201500.


13. Texas Medical Association. EMR implementation guide - online course instruction [Internet]. Austin (TX): Texas Medical Association; c2013. cited at 2015 Apr 15. Available from: http://www.texmed.org/Template.aspx?id=6188

14. MMIC Group. The Certified Electronic Medical Record Risk Management Premium Credit [Internet]. Minneapolis (MN): MMIC Group; 2014. cited at 2015 Apr 15. Available from: http://mmicgroup.com/pdf/EHR_Application.pdf

15. King P. Can electronic medical records help to decrease malpractice insurance costs? [Internet]. [place unknown]: netdoc.com; 2010. cited at 2015 Apr 15. Available from: http://www.netdoc.com/Physician-Practice-Articles/General-Medical-Practice/Can-Electronic-Medical-Records-Help-to-Decrease-Malpractice-Insurance-Costs?/

16. Lee J, Dowd B. Effect of health information technology expenditure on patient level cost. Healthc Inform Res 2013;19(3):215-221. PMID: 24175120.



17. Reiter KL, Song PH. The role of financial market performance in hospital capital investment. J Health Care Finance 2011;37(3):38-50. PMID: 21528832.


18. McCullough JS. The adoption of hospital information systems. Health Econ 2008;17(5):649-664. PMID: 18050147.


19. Gowrisankaran G, Town RJ. Estimating the quality of care in hospitals using instrumental variables. J Health Econ 1999;18(6):747-767. PMID: 10847933.


20. Lave JR, Pashos CL, Anderson GF, Brailer D, Bubolz T, Conrad D, et al. Costing medical care: using Medicare administrative data. Med Care 1994;32(7 Suppl):JS77-JS89. PMID: 8028415.


21. Hayes KJ, Pettengill J, Stensland J. Getting the price right: Medicare payment rates for cardiovascular services. Health Aff (Millwood) 2007;26(1):124-136. PMID: 17211021.


22. Gapenski LC. Healthcare finance: an introduction to accounting and financial management. 5th ed. Chicago (IL): Health Administration Press; 2012.

23. Office of Statewide Health Planning & Development. Case Mix Index [Internet]. Sacramento (CA): Office of Statewide Health Planning & Development, State of California; 2014. cited at 2015 Apr 15. Available from: http://www.oshpd.ca.gov/HID/Products/PatDischarge-Data/CaseMixIndex/

25. Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res 2010;10:231PMID: 20691097.



26. DesRoches CM, Campbell EG, Rao SR, Donelan K, Ferris TG, Jha A, et al. Electronic health records in ambulatory care--a national survey of physicians. N Engl J Med 2008;359(1):50-60. PMID: 18565855.


27. Vishwanath A, Scamurra SD. Barriers to the adoption of electronic health records: using concept mapping to develop a comprehensive empirical model. Health Informatics J 2007;13(2):119-134. PMID: 17510224.


28. KevinMD. Do electronic medical records decrease liability risk? [Internet]. [place unknown]: KevinMD.com; 2009. cited at 2015 Apr 15. Available from: http://www.kevinmd.com/blog/2009/12/electronic-medicalrecords-decrease-liability-risk.html

29. Victoroff MS, Drury BM, Campagna EJ, Morrato EH. Impact of electronic health records on malpractice claims in a sample of physician offices in Colorado: a retrospective cohort study. J Gen Intern Med 2013;28(5):637-644. PMID: 23192449.


-
METRICS

- Related articles in Healthc Inform Res
-
Healthcare Information Technology: A Systematic Mapping Study2023 January;29(1)
Health Information Technology Trends in Social Media: Using Twitter Data2019 April;25(2)
Public Acceptance of a Health Information Exchange in Korea2018 October;24(4)
Association between Health Information Technology and Case Mix Index2017 October;23(4)
Steps in Moving Evidence-Based Health Informatics from Theory to Practice2016 October;22(4)