1. Bhandari G, Snowdon A. Adoption of open source software in healthcare. In: Phillips-Wren G, Jain LC, Nakamatsu K, , editors. Advances in intelligent decision technologies. Heidelberg: Springer; 2010. p. 365-372.

2. Saebi T, Foss NJ. Business models for open innovation: matching heterogeneous open innovation strategies with business model dimensions. Eur Manag J 2015;33(3):201-213.

3. Morgan L, Finnegan P. Benefits and drawbacks of open source software: an exploratory study of secondary software firms. In: Feller J, Fitzgerald B, Scacchi W, , editors. Open source development, adoption and innovation. Boston (MA): Springer; 2007. p. 307-312.

4. Reynolds CJ, Wyatt JC. Open source, open standards, and health care information systems. J Med Internet Res 2011;13(1):e24. PMID:
21447469.



5. Ratib O, Rosset A, Heuberger J. Open Source software and social networks: disruptive alternatives for medical imaging. Eur J Radiol 2011;78(2):259-265. PMID:
21444166.


6. Zaidan AA, Zaidan BB, Al-Haiqi A, Kiah ML, Hussain M, Abdulnabi M. Evaluation and selection of open-source EMR software packages based on integrated AHP and TOPSIS. J Biomed Inform 2015;53:390-404. PMID:
25483886.


7. Goldwater JC, Kwon NJ, Nathanson A, Muckle AE, Brown A, Cornejo K. Open source electronic health records and chronic disease management. J Am Med Inform Assoc 2014;21(e1):e50-e54. PMID:
23813566.


8. Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med 2010;363(6):501-504. PMID:
20647183.


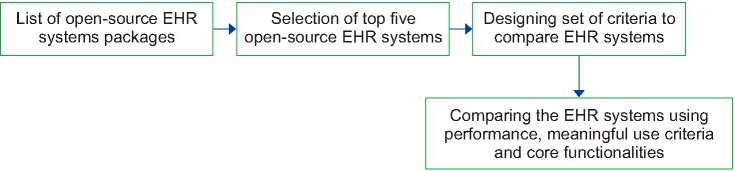
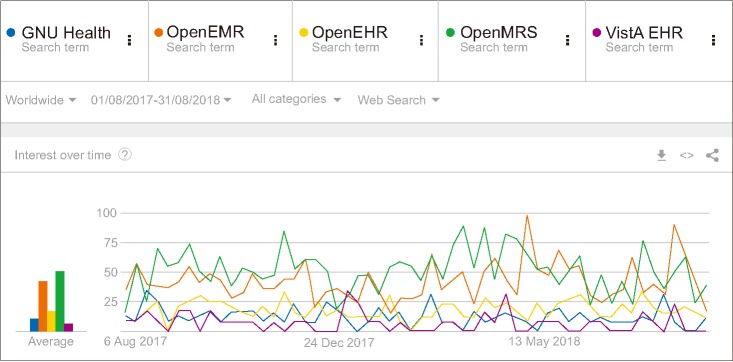
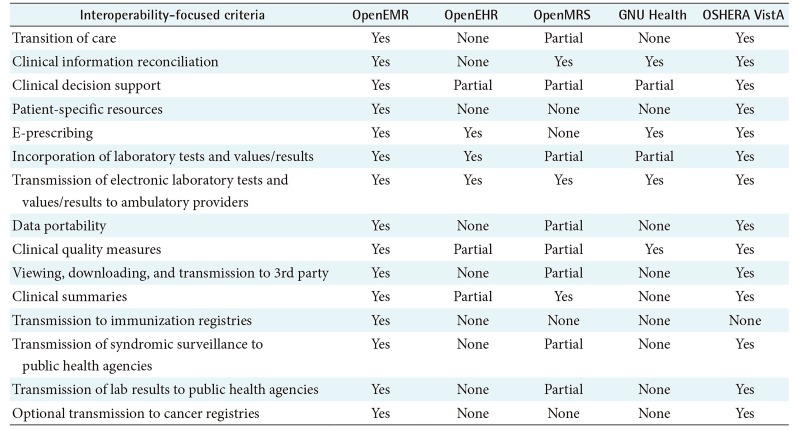
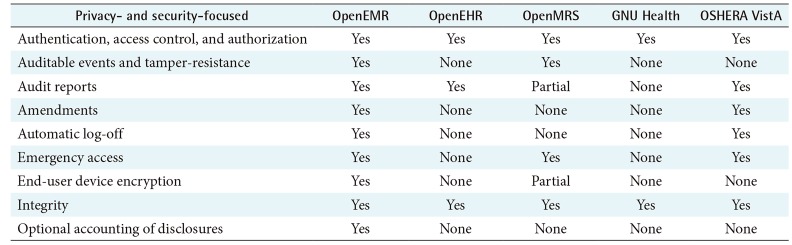
9. de Abajo BS, Ballestero AL. Overview of the most important open source software: analysis of the benefits of OpenMRS, OpenEMR, and VistA. In: Rodrigues JJ, de la Torre-Diez I, de Abajo BS, , editors. Telemedicine and e-health services, policies, and applications: advancements and developments. Hershey (PA): IGI Global; 2012. p. 315-346.

10. Tripathi M. EHR evolution: policy and legislation forces changing the EHR. J AHIMA 2012;83(10):24-29.

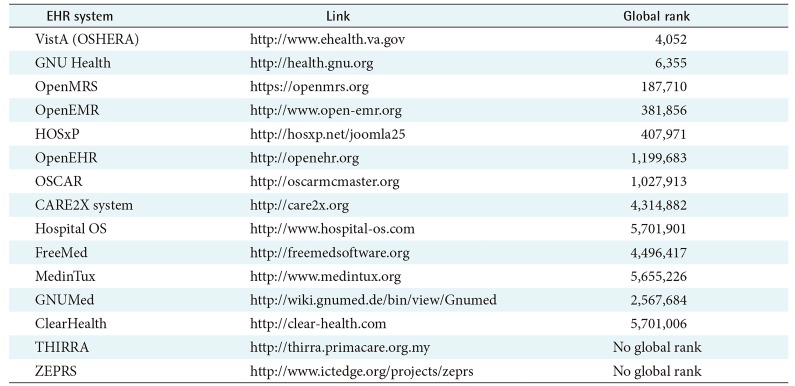
11. Jones B, Yuan X, Nuakoh E, Ibrahim K. Survey of open source health information systems. Health Inform 2014;3(1):23-31.

12. Karopka T, Schmuhl H, Demski H. Free/Libre open source software in health care: a review. Healthc Inform Res 2014;20(1):11-22. PMID:
24627814.



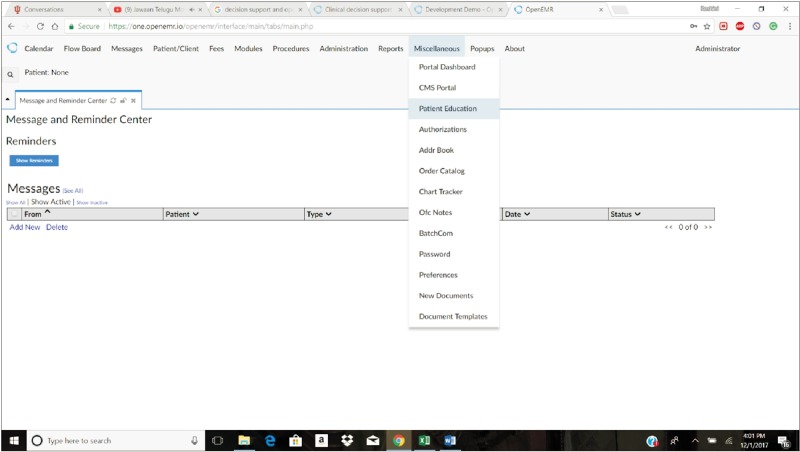
13. Kiah ML, Haiqi A, Zaidan BB, Zaidan AA. Open source EMR software: profiling, insights and hands-on analysis. Comput Methods Programs Biomed 2014;117(2):360-382. PMID:
25070757.


14. Kashfi H. An openEHR-based clinical decision support system: a case study. Stud Health Technol Inform 2009;150:348PMID:
19745328.


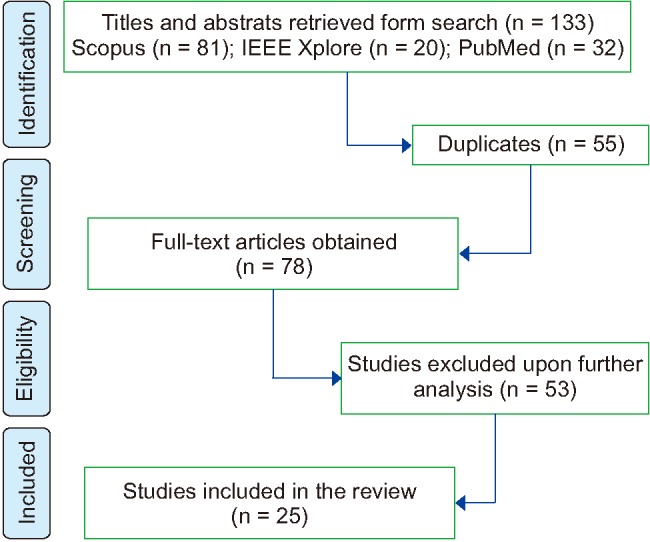
15. Syzdykova A, Malta A, Zolfo M, Diro E, Oliveira JL. Open-source electronic health record systems for low-resource settings: systematic review. JMIR Med Inform 2017;5(4):e44. PMID:
29133283.



16. Alsaffar M, Yellowlees P, Odor A, Hogarth M. The state of open source electronic health record projects: a software anthropology study. JMIR Med Inform 2017;5(1):e6. PMID:
28235750.



17. Oza S, Jazayeri D, Teich JM, Ball E, Nankubuge PA, Rwebembera J, et al. Development and deployment of the OpenMRS-Ebola electronic health record system for an Ebola treatment center in Sierra Leone. J Med Internet Res 2017;19(8):e294. PMID:
28827211.