|
 |
- Search
| Healthc Inform Res > Volume 24(1); 2018 > Article |
Abstract
Objectives
Developments in advanced technology have unlocked an era of smart health, transforming healthcare practices inside and outside hospitals for both medical staff and patients. It is now possible for patients to collect detailed health data using smartphones and wearable devices, regardless of their physical location or time zone. The use of these patient-generated data holds great promise for future healthcare advancements in many ways; however, current strategies for smart-health technologies tend to focus on the smartness of the technology itself and on managing a particular disease or condition. Moreover, opportunities for people within the healthcare system to experience the benefits of these innovations are still limited.
Methods
An expert workshop was held to discuss the current limitations of smart health, where each expert gave a presentation on their particular expertise, followed by an exchange of ideas for the purpose of drawing conclusions.
Results
‘Smartness’ should not be the ultimate value for patients using smart technologies; instead of focusing on individual smart devices, we should consider the space around people and their relation to each object so that the combination of space and objects brings an ‘enchanted’ experience to user.
Conclusions
An ‘enchanted’ experience can only be possible when monitoring provides the user with a comfortable life and satisfies their needs and desires sufficiently. Only when the novelty of the device's smartness effectively connects people with the space around them and focuses on human desires can it be cost effective and value creating.
Advancements in information and communications technologies (ICT) have transformed the healthcare industry in the last decade affording patients higher accessibility, efficiency, and satisfaction in regard to their interactions with the healthcare system [12]. Hospitals now have networks that enable patients to interact efficiently and conveniently with health-services professionals: sign-in kiosks register patients and help them navigate the system, monitors in waiting areas keep patients informed of appointments, and computerized scales and blood pressure machines enable self-assessment of patients without overburdening nurses. Patient medical histories are managed through the Electronic Medical Record (EMR) system instead of paper charts, and patients also can review their health records through mobile applications [345].
Widely deployed smartphones and wearable devices, as well as the emergence of Internet of Things (IoT) sensor technologies, make it possible for patients to collect detailed health data outside of hospitals, enabling ‘pervasive healthcare’—in other words, ‘healthcare to anyone, anytime, and anywhere by removing locational, time and other restraints while increasing the coverage and quality’ [6]. These technologies hold the promise of reducing costs by providing healthcare away from hospitals and closer to home, while centralized healthcare repositories can receive increasingly detailed data from patients enabling efficiency gains in both diagnosis and treatment [7].
As a result, a plethora of healthcare applications are being introduced to healthcare markets. In addition, ‘personalized preventative health coaches’ (digital health advisors) will emerge to help clients manage chronic and diet-related illnesses through those apps [8]. There are more than 318,000 health apps and more than 340 consumer wearable devices worldwide with two main service sector categories: wellness management and health-condition management [9]. Although general-wellness apps comprise the majority of these, apps focused on health-condition management account for an increasing share, currently at 40% of all health apps.
Wellness-management apps often facilitate the tracking and modification of fitness behaviors, lifestyle, stress management, and diet (such as weight loss, food diary, stress management, smoking cessation, or alcohol moderation) [10111213]. Health-condition management apps supply information on diseases and conditions, enable access to care, and enable treatment protocols—for example, diabetes self-management, atrial fibrillation management, or mental disorder treatment [141516].
Although it is inside and outside of hospitals, ICT has become quite advanced, and the current system is centered around managing a particular condition using smartphones or wearable devices, and people's experiences with healthcare are limited. Individual data sets reflect only specific aspects of a person's status; for instance, glucose meters provide only a limited scope of a person's overall health [17]. In addition, the retention rates of mobile apps tend to drop after the initial phase [18], and wearable technologies such as smart watches require initiative from users, which often results in a loss of interest over time [1920].
To truly integrate technology and revolutionize healthcare, we conducted a small workshop to review the current status of smart health technology and to exchange ideas. A total 20 people coming from various healthcare related expertises (e.g., clinicians, medical informaticians, IT experts, medical law professionals, etc.) attended the initial workshop where seven experts presented the topic and prospective from their particular area of expertise. An additional discussion session was held among the authors after the initial drafting of the paper to reach a consensus on the proposed terms and concept.
Based on the ideas exchanged at the workshop, we propose a vision of healthcare in an ‘enchanted life space’, where the focus of healthcare moves away from specialized devices and gadgets and towards directly influencing the space around people through holistic engagement. To achieve this vision, where people consider healthcare as part of their lifestyle and retain sustainable engagement with it, such a system must offer additional benefits such as boosts to happiness, healthiness, emotional support, and empathy in addition to the ‘smartness’ of the technology itself.
The remainder of this paper is organized as follows. First, we define the concepts of human desire and the ‘enchanted’ life space and then present a potential scenario in which healthcare is implemented, and the enchanted components are embedded in a person's life space. Next, we discuss the current limitations of the technology and the requirements for creating the future of healthcare through data integration, standards, and legal perspectives. Finally, there is a discussion.
As digital technology evolved, a belief arose that analog would be replaced completely by digital. However, in reality, sales of paper books have increased despite the appearance of the e-book, and people still choose to wear an analog watch over a digital or smartwatch. Furthermore, a new type of medium has also been gaining popularity, which combines the perceived emotionality of analog with the digital technology, such as a smartphone picture-taking app that mimics a film camera mechanism [21]. This phenomenon demonstrates that, while in some ways advances in digital technology make people's lives easier, faster, and more convenient, many individuals still have a desire and sense of nostalgia for analog, even though they may deal with some inconvenience and slowness. This means that, when designing any service using technology, in addition to utilizing innovative technology, a necessary condition is satisfying human desire.
David Rose divided such human drives into six categories and introduced the concept of the ‘enchanted object’, the embodiment of which connects six human desires [22]. People wish for six things that enchanted objects satisfy: omniscience (desire to know all), telepathy (desire for human connection), safekeeping (desire to protect or be protected), immortality (desire to live a long, healthy, and quantified life), teleportation (desire to move effortlessly), and expression (desire to create, make, and play). One of the ‘enchanted objects’ Rose developed for healthcare is Vitality's GlowCaps [23], a wireless pill-bottle cap designed to improve medication adherence through smart packaging, reminders, reports, and rewards. Ordinary pill bottles were ‘enchanted’ by embedding wireless technology so that a glow would remind you when to take your medication. This has not only helped with medication adherence but additionally, led to other healthy behaviors such as smoking cessation, weight loss, and ending alcohol abuse.
This kind of enchantment can also be expanded to one on a larger scale which, in our case, is the creation of a ‘life space’—any space or environment where people live and spend time, such as the home, workplace, their car, the city they live in, or even a hospital. As opposed to focusing on individual enchanted objects, we consider the space around people and their relation to each object. In this way, the combination of space and objects brings an enchanted experience to the users. To achieve this, a suitable balance must be found, in such a way as to not hinder everyday human activities like working, sleeping, driving, etc., but yet still allows the collection of sufficient information as the basis for the effective provision of personalized healthcare services.
The main differences between the ‘enchanted life space’ and the current status of smart health would be its ability to reflect human desire and emotion as well as the technological advantage of smart devices themselves. A smart home, for example, would be composed of various IoT sensors and devices (e.g. a smart thermostat or lighting system, networked security cameras, etc.), which work harmoniously to provide convenience and monitoring capabilities within the home. If it was an enchanted home, on the other hand, its inhabitants would be in immersed within an atmosphere filled with comfort, affection, and memories, in addition to the ‘smartness’ of the technology. An ordinary looking antique rocking chair might be equipped with an accelerometer and gyroscope sensors that detects the rocking patterns of a given user, extracting motor health conditions. Not only would the rocking chair monitor the user's health status, but it could also serve as a medium that recalls the memory of loved one by manipulating the lighting and music playing throughout the home whenever the user started rocking on chair, thus provoking reminisce and nostalgia.
In addition to smartphones, wearable devices, or medical devices, which are carried or attached to the human body, IoT sensors are also being developed. IoT sensors gather human status data via indirect methods, such as wall-mounted sensor devices that detect human sleep activity using radio signals [24]. This kind of technology has great potential for providing healthcare in various types of space because it enables continuous sensing and data exchanges between spaces rather than just being limited to one location and time (Figure 1).
For example, consider a day in the life of an IT developer who is obese due to irregular eating habits and lack of exercise. Living in an enchanted life space may start with a self-check in the bathroom after waking up, in which the bathroom mirror displays the duration and quality of last night's sleep while a bath mat underneath him measures his current weight and body temperature. A sensor embedded in his bed tracks his sleep, and today, a warning notification is displayed in the mirror while he is washing his face stating that his sleep apnea is getting worse because of his obesity and suggests that he makes a doctor's appointment. The system reviews his work and personal calendars and automatically schedules an appointment with his primary physician in 2 days' time. As he finishes wiping his face with a towel, the mirror displays an image of a fitter, in-shape version of himself in a month if he follows a new diet-and-exercise plan.
He leaves in a hurry for work and gets into his car to commute, which takes 30 minutes. While driving, a sensor embedded in the steering wheel detects his heart rate and rhythm, and the dashboard reminds him of this morning's warning sign about his health condition, which encourages him to decide to start working out from now on. Halfway through his commute, an abnormality is detected in his electrocardiogram (ECG), and the artificial intelligence (AI) agent suggests that he visits a nearby hospital right away.
As he arrives at the hospital, the hospital staff have already reviewed his health record along with his previous night's sleep report and the ECG results from while he was driving, which enables the staff to order more tests related to his heart condition already. It turns out that his heart has been under extra stress due to his obesity and increased blood pressure, which have been affecting his sleep quality as well. The doctor prescribes medication along with an exercise plan and suggests further routine follow ups through virtual appointment sessions at home.
He decides to take a day off from work and notifies the company. The hospital also sends the relevant information pack for applying for a treatment plan at the workplace (e.g., specialized meal plan, modified work schedule, etc.). As he steps back into his house, he receives an incoming video call from his parents, who are living in another country. They have been notified by the hospital, and he feels relieved and better already as he talks to his family.
The relevant content and context for describing a person are found not only in medical settings but also across all the life spaces in which the subject inhabits throughout his or her life. Effectively and appropriately collecting, processing, and integrating these to derive and infer knowledge will be at the core of future health- and disease-management services.
To achieve goals such as accurate risk assessment for disease occurrence, early prediction of disease aggravation and optimization of interventions by evaluating an individual's multifaceted health status is necessary to develop highly detailed, longitudinal, and multi-parametric models. This will require fully utilizing data from various monitoring devices and systems. Developing a model for this holistic view of health and disease management, however, presents a number of challenges related to individual data collection and integration techniques. In general, biomedical data—especially longitudinal, multi-parametric data—have problems with high-dimensionality, heterogeneity, temporal dependency, sparsity, irregularity, noisiness, ambiguity, and data redundancy [25], while data integration is complicated by concerns over privacy and multimodal harmonization [26].
The complexity of using data in these ways, along with the desirability of the underlying goals, has prompted researchers to attempt various alternative approaches instead of traditional analytical methodologies. Various techniques have been recently introduced, one famous example being ‘deep learning’ in which new methodologies are applied in a stepwise or complex manner rather than a single methodology. Unlike conventional machine learning methodologies, deep learning applies various concepts and algorithms that are suitable for analyzing the high-dimensionality, heterogeneity, and temporal dependency of longitudinal, multi-parametric data sets, data integration, and multimodal harmonization.
For these reasons, a recent study has studied proposed applications of this new methodology [25] by analyzing medical images, EMR, genomics, mobile data, and multimodal data-based models. At the same time, this does not represent a silver bullet that will solve all the problems we face, and it also presents its own sets of unique challenges, such as understanding the model's explanatory power. Above all, no clear solutions or countermeasures have been proposed to answer the fundamental question of how to collect, process, and refine the data underlying the modeling bases. The robust construction of the most basic units making up the model is critical to the final model. Until that is accomplished, there is no way that the model's reliability, accuracy, reproducibility, and scalability can be guaranteed.
Platform research is actively being carried out to collect and analyze personal health information so as to utilize it for medical services. There is a trend toward developing standards for technology and information integration that can be commonly applied in the field of medical information and medical devices based on the IoT.
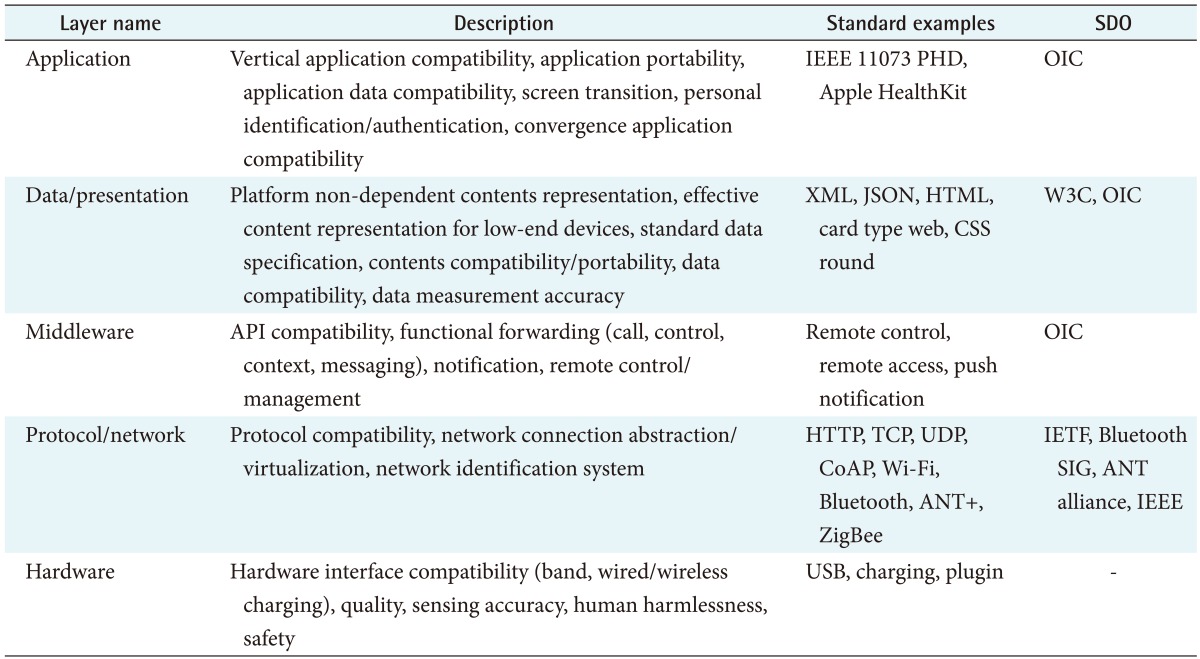
To exchange and utilize medical information and medical device data, standards development organizations such as the International Organization for Standardization (ISO), Health Level Seven International (HL7), Institute of Electrical and Electronics Engineers (IEEE), and International Electrotechnical Commission (IEC) are developing various standards for interoperability. Recently, the Telecommunication Technology Association (TTA) constructed a smart wearable application interoperability reference model [27] to enable the organization of these standards by referring to the Open Systems Interconnection (OSI) 7-layer model (Table 1). To ensure the interoperability of IoT-based data, for each layer, a description from hardware to application, standard examples developed, and standard development organizations were listed.
It is not easy for developers of smart wearables to apply existing standards based on usage because these standards span many different areas of technology (Figure 2). Various use cases for medical information and devices are being defined to adapt to standards more quickly, and there are organizations that provide a standardized application method and an open platform tailored to each use case. These organizations are developing smart wearable standards and organically applying those standards. Representative companies include the Open Connectivity Foundation (OCF), which aims to integrate the IoT standards through collaboration among various industries and to help developers and companies develop seamless IoT solutions.
Although human intervention is minimized in IoT-based healthcare (i.e., passive data) for the enchanted life space, it is still a human-friendly space. Under the current regulation frame, the collection and utilization of data collected throughout those spaces requires the active informed consent of subjects. Data that typically utilize wearable technology or mobile devices to capture and chronicle an individual's life is often referred to as ‘lifelog data’ (Figure 2); however, there are no independent regulations for lifelog data—the distinction between personally identifiable data and non-personally identifiable data is vague, and there are still several legal accountability issues to overcome [28].
Information generated from multiple spaces is required for providing a personalized service, and because universal regulation does not exist for such services, several acts and regulations must be taken into consideration. To operate healthcare using the enchanted life space in South Korea, it is necessary to comply with the following laws and regulations presented in Table 2. This classification specifies the necessary statutory requirements to be complied with when handling various sorts of data under the name of lifelog in the life space.
Modern society is led by consumption rather than production, which means that consumer values are more important than the needs of the industry itself [29]. Currently, there are several kinds of added values offered by the smart industry; however, they do not seem to be concordant with consumer values. How can a smart watch, a smart car, or a smart home satisfy human desires? Mastering this could decide the success or failure of a smart technology.
Although we have introduced six human desires [22], they are not the result of a consensus among healthcare stakeholders; therefore, a broader frame is necessary to evaluate smart technologies from the perspective of a life space. For example, these desires could be considered concurrently with the six aims for the improvement of healthcare quality (i.e., safe, effective, patient centered, timely, efficient, and equitable) outlined by the Institute of Medicine (IOM) [30]. Until then, the smart technology industry cannot truly improve quality of life in the healthcare domain.
Although there are numerous smart devices (e.g., smart watches and smart cars), not all of them can satisfying human desires or monitor the user's health status (e.g., heart rate, activity, stress level, mood, etc.). Smart devices and technologies—wearables, embedded, and touchless—are limited to their sensors and hardware specifications. Thus, asking the question which kinds of smart devices are most suitable for satisfying human desires is essential. The roles of smart devices should be discussed—based on their sensors and hardware specifications, users' behaviors in their spaces, and people's values and desires for them at any given time—especially with respect to good health. By establishing the roles of smart devices and their current status, we can better determine any missing links to provide living space health services without disconnection.
Healthcare for the life space requires a variety of data and services: personal genomes, clinical data, behavioral information, lifelogs, and health insurance. Smart technology cannot gather all the healthcare data; it must be connected and integrated with existing and emerging healthcare services. The integration and interface framework of all healthcare services for life spaces should be developed including data collection and analysis, standardization, and legal issues. Research related to this issue is desperately needed in order for smart devices to become better settled in routine healthcare.
There is always the concern of privacy issues when using technology to collect data and to provide a service based on said data. Monitoring a variety of places constantly may ultimately be viewed as monitoring the patterns of daily life, and this kind of surveillance has a number of negative implications. On a basic level, the legality and the protection of individual rights should be considered. However, going one step further, people should be able to accept and embrace the concept of healthcare services in an enchanted space of life. This can only be possible when monitoring provides the user with a comfortable life and satisfies their needs and wants. It is important to think in terms of security; however, it is even more crucial to focus on the patient's desires and to design devices to meet those desires.
There are a variety of services currently available that focus on smart devices; however, the ultimate goal for people using these technologies is their own health and desire, not for the device and ‘smartness’ itself. It is necessary to build a system where smart devices and the related technology are geared to deliver happiness; not the other way around where, as machines become smarter, people just become more reliant on technology. Only when the novel smartness of a device effectively connects people with the space around them and focuses on human desires can this be cost effective and value creating.
Acknowledgments
The authors would like to express their gratitude to all members of the Health Innovation Big Data Center and Clinical Information Strategy Team (Research Information Unit) for organizing the workshop and providing support to complete this work.
References
1. Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144(10):742-752. PMID: 16702590.


2. Akesson KM, Saveman BI, Nilsson G. Health care consumers' experiences of information communication technology: a summary of literature. Int J Med Inform 2007;76(9):633-645. PMID: 16931133.


3. Johns Hopkins Medicine. Hartlove B. Patient check-in kiosk goes live at the Johns Hopkins Medical Laboratory @ White Marsh [Internet]. Baltimore (MD): Johns Hopkins Medicine; 2014. cited at 2018 Jan 10. Available from: http://apps.pathology.jhu.edu/blogs/pathology/patient-check-in-kiosk-goes-live-at-the-johns-hopkinsmedical-laboratory-white-marsh

4. Fuhrer P, Guinard D. Building a smart hospital using RFID technologies: use cases and implementation. Fribourg, Switzerland: Department of Informatics, University of Fribourg; 2006.

5. Park JY, Lee G, Shin SY, Kim JH, Han HW, Kwon TW, et al. Lessons learned from the development of health applications in a tertiary hospital. Telemed J E Health 2014;20(3):215-222. PMID: 23909863.



6. Varshney U. Pervasive healthcare computing: EMR/ EHR, wireless and health monitoring. Boston (MA): Springer; 2009.

7. Ericsson. From healthcare to homecare [Internet]. Stockholm, Sweden: Ericsson; c2017. cited at 2018 Jan 10. Available from: https://www.ericsson.com/en/networked-society/trends-and-insights/consumerlab/consumer-insights/reports/transforming-healthcarehomecare

8. Dimitrov DV. Medical Internet of Things and big data in healthcare. Healthc Inform Res 2016;22(3):156-163. PMID: 27525156.



9. IQVIA Institute. The growing value of digital health in the UK: evidence and impact on human health and the healthcare system [Internet]. Durham (NC): IQVIA Institute; c2017. cited at 2018 Jan 10. Available from: https://www.healthcare.digital/single-post/2017/11/08/The-Growing-Value-of-Digital-Health-in-the-UK

10. Carter MC, Burley VJ, Nykjaer C, Cade JE. Adherence to a smartphone application for weight loss compared to website and paper diary: pilot randomized controlled trial. J Med Internet Res 2013;15(4):e32. PMID: 23587561.



11. Laurie J, Blandford A. Making time for mindfulness. Int J Med Inform 2016;96:38-50. PMID: 26965526.


12. Bricker JB, Mull KE, Kientz JA, Vilardaga R, Mercer LD, Akioka KJ, et al. Randomized, controlled pilot trial of a smartphone app for smoking cessation using acceptance and commitment therapy. Drug Alcohol Depend 2014;143:87-94. PMID: 25085225.



13. Gonzalez VM, Dulin PL. Comparison of a smartphone app for alcohol use disorders with an Internet-based intervention plus bibliotherapy: a pilot study. J Consult Clin Psychol 2015;83(2):335-345. PMID: 25622202.



14. Petersen M, Hempler NF. Development and testing of a mobile application to support diabetes self-management for people with newly diagnosed type 2 diabetes: a design thinking case study. BMC Med Inform Decis Mak 2017;17(1):91PMID: 28651639.



15. Guo Y, Chen Y, Lane DA, Liu L, Wang Y, Lip GYH. Mobile health technology for atrial fibrillation management integrating decision support, education, and patient involvement: mAF App trial. Am J Med 2017;130(12):1388-1396.e6. PMID: 28847546.


16. Gravenhorst F, Muaremi A, Bardram J, Grunerbl A, Mayora O, Wurzer G, et al. Mobile phones as medical devices in mental disorder treatment: an overview. Pers Ubiquitous Comput 2015;19(2):335-353.

17. Rodbard D. Continuous glucose monitoring: a review of successes, challenges, and opportunities. Diabetes Technol Ther 2016;18(Suppl 2):S3-S13.

18. Hsiao CH, Chang JJ, Tang KY. Exploring the influential factors in continuance usage of mobile social apps: satisfaction, habit, and customer value perspectives. Telemat Inform 2016;33(2):342-355.

19. Jeong H, Kim H, Kim R, Lee U, Jeong Y. Smartwatch wearing behavior analysis: a longitudinal study. Proc ACM Interact Mob Wearable Ubiquitous Technol 2017;1(3):60.

20. Lazar A, Koehler C, Tanenbaum J, Nguyen DH. Why we use and abandon smart devices Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing; 2015 Sep 7–11. Osaka, Japan; p. 635-646.

21. Apple App Store. Gudak Cam application by Screw Bar Inc. [Internet]. Cupertino (CA): Apple Inc.; c2016. cited at 2018 Jan 10. Available from: https://itunes.apple.com/us/app/gudak-cam/id1237692856

22. Rose D. Enchanted objects: design, human desire, and the Internet of Things. New York (NY): Simon and Schuster; 2014.

23. Reese PP, Kessler JB, Doshi JA, Friedman J, Mussell AS, Carney C, et al. Two randomized controlled pilot trials of social forces to improve statin adherence among patients with diabetes. J Gen Intern Med 2016;31(4):402-410. PMID: 26585957.


24. Zhao M, Yue S, Katabi D, Jaakkola TS, Bianchi MT. Learning sleep stages from radio signals: a conditional adversarial architecture Proceedings of the 34th International Conference on Machine Learning (PMLR); 2017 Aug 6–11. Sydney, Australia; p. 4100-4109.

25. Miotto R, Wang F, Wang S, Jiang X, Dudley JT. Deep learning for healthcare: review, opportunities and challenges. Brief Bioinform 2017 5 6 [Epub]. PMID: 10.1093/bib/bbx044.

26. Johnson AE, Ghassemi MM, Nemati S, Niehaus KE, Clifton DA, Clifford GD. Machine learning and decision support in critical care. Proc IEEE Inst Electr Electron Eng 2016;104(2):444-466. PMID: 27765959.



27. Telecommunications Technology Association. Smart wearable application interoperability reference model [Internet]. Seongnam, Korea: Telecommunications Technology Association; 2015. cited at 2018 Jan 10. Available from: http://www.tta.or.kr/data/ttas_view.jsp?rn=1&pk_num=TTAK.KO-06.0412

Figure 1
Collection and integration of an individual's health data from various devices and sensors in the life space.

Figure 2
Lifelog data may utilize and communicate with both retrospective and prospective data. The acquisition of informed consent will be required at the beginning of any prospective data collection.