Barriers in Health Information Systems and Technologies to Support Maternal and Neonatal Referrals at Primary Health Centers
Article information
Abstract
Objectives
This study explored health workers’ perceptions and experiences regarding the maternal and neonatal referral system, focusing on barriers of health information systems and technologies (IS/IT) at primary health centers (PHCs) in South Tangerang, Indonesia.
Methods
This qualitative study was conducted using semi-structured interviews, which were conducted at the South Tangerang District Health Office and three PHCs. Interviews were conducted with nine participants responsible for maternal and neonatal referrals in their organizations. The data were analyzed using qualitative content analysis.
Results
In South Tangerang, the Primary Health Care Information System (SIMPUS) is used to register patients and record data on medical treatment. To facilitate referrals, the PHCs currently use the Integrated Referral Information System (SISRUTE), P-Care, and the Integrated Emergency Management System (SPGDT). The following four IS/IT barriers to support maternal and neonatal referrals were found: technology, human resources, organizational support, and the referral process and implementation.
Conclusions
The barriers in technology, human resources, and organizational support cause problems in the maternal and neonatal referral process and in the implementation of referrals. Barriers to referrals can influence patients’ ability to receive appropriate care in a timely fashion and lead to inefficiency in maternal and neonatal referrals. This study contributes knowledge about IS/IT implementation in maternal and neonatal referral systems and provides recommendations to health regulators and application developers for the implementation of IS/IT in Indonesia.
I. Introduction
The referral system is an essential element of maternal and neonatal health [1]. Some developing countries have implemented health information systems or technologies (IS/IT) to support communication, transportation, or documentation in maternal and neonatal health referrals [2]. Previous studies about these technologies have primarily focused on design [3] and the benefits of IS/IT to support referrals [4,5]. However, there is a lack of research exploring users’ perspectives on using technologies to support maternal and neonatal referrals.
The effective deployment of IS/IT requires both organizational support and users’ ability to use technologies [6]. Unreliable infrastructure, lack of interoperability of systems, lack of regulations, and lack of healthcare workers’ commitment are common barriers to IS/IT implementation in developing countries [7,8]. Barriers to IS/IT can cause inefficiency in maternal and neonatal referrals [2]. Discussing users’ perspectives on current IS/IT use can determine future improvements for maternal and neonatal referral systems.
Limited research has been conducted on technologies to support maternal and neonatal referrals in Indonesia, which is a developing country. Moreover, research on the referral system in Indonesia still focuses on its implementation in hospitals, and little research has been conducted at primary health centers (PHCs) [9]. PHCs play an essential role as gatekeepers for curative and public health services [10] and link patients to Indonesia’s referral system [11]. Some PHCs in districts/cities in Indonesia still process data manually [12], and there is rarely a designated person to manage health information systems [10]. The Indonesian government has developed IS/IT systems to support maternal and neonatal referral, such as the Information and Communication System for Maternal and Neonatal Referral Networks (SijariEMAS) and SMSBunda—a text messaging service for pregnant women and postnatal mothers [13]. However, these systems did not work effectively in several regions because they did not consider each region’s specific characteristics [13].
The district of South Tangerang in Banten Province is an urban area in Indonesia that is currently developing an integrated referral system focusing on individual health referrals [14]. In Indonesia, maternal and neonatal referral health systems have different guidelines and requirements from those of individual health referrals [15]. This study explored health management and health workers’ experiences with the maternal and neonatal referral system, focusing on IS/IT barriers at PHCs in South Tangerang.
II. Case Description
1. Participant Selection
The South Tangerang has 25 PHCs in seven sub-districts and one public hospital [16]. This study was conducted at three PHCs (Pamulang, Pondok Benda, and Pisangan) and the South Tangerang District Health Office (DHO) as the regulator of PHCs. These PHCs were selected based on a recommendation from the DHO and were considered to have exemplary IT implementation. This study used purposive sampling to select participants with the best knowledge concerning the research topic. The participants from the DHO worked in the family health section and the health human resources section, while the participants from the PHCs were workers in the maternal and child health section and administrative staff (Table 1).
2. Data Collection
The authors conducted semi-structured interviews between April and September 2019, with an average duration of 30–45 minutes. The interview questions were related to the maternal and neonatal referral process and health IS/IT that can support referrals (Table 2). Interviews were recorded and transcribed for analysis.
3. Data Analysis
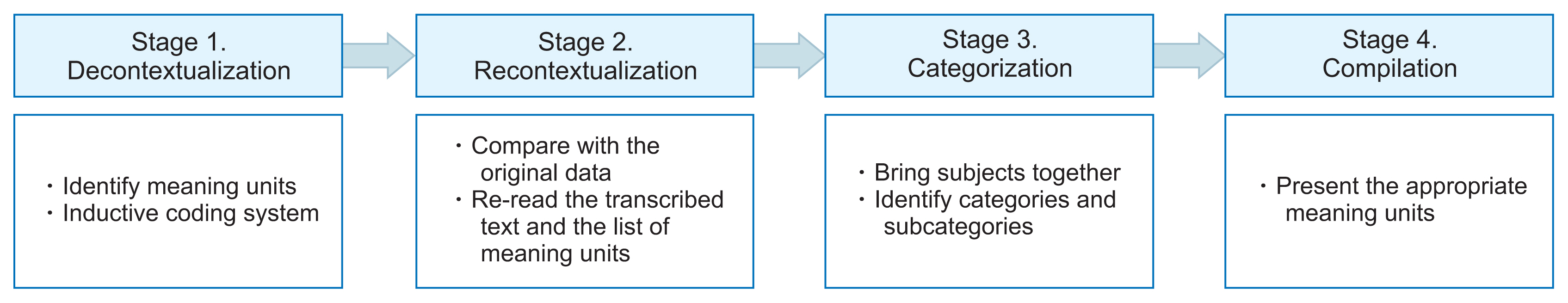
This study used content analysis, consisting of decontextualization, recontextualization, categorization, and compilation [17] (Figure 1). In the decontextualization step, the authors read each transcribed text, broke the text into smaller meaning units, and created codes inductively [17]. In recontextualization, the authors compared the original data by rereading the transcribed text and the list of meaning units to check whether there are unmarked texts to be included. In the categorization step, the authors identified the categories and sub-categories from the meaning units. Finally, the authors choose the appropriate meaning units presented in the running text as quotations [17]. The authors did not find new codes and themes after analyzing interview results from five participants. The remaining interview results confirmed the answers of the other participants. The first author conducted the analysis, while others reviewed the process and categorization to ensure its trustworthiness.
4. Maternal and Neonatal Referral System in South Tangerang
After a patient arrives at the maternal and child health section at a PHC, a health worker examines the patient. The health worker refers the patient to a hospital if complications are identified. The health worker communicates with the hospital to check available rooms and equipment and inform the hospital of the patient’s condition. Furthermore, The health worker calls an ambulance for the patient, but the health worker also accompanies the patient in the ambulance.
In South Tangerang, the Primary Health Care Information System (SIMPUS) is used to register patients, record diagnoses, and report activities to the DHO [18]. For referral, PHCs use the Integrated Referral Information System (SISRUTE) for information exchange [19] and P-Care to generate referral letters for patients with coverage through the Social Health Insurance Administration Body (BPJS Kesehatan) [20]. SijariEMAS was replaced by one system, that is SP-GDT (the Integrated Emergency Management System). SP-GDT is the only emergency call center system in the South Tangerang area [21]. Table 3 presents the IS/IT used in South Tangerang.
5. Results
Barriers to IS/IT to support maternal and neonatal referrals consisted of technology, human resources, organizational support, and the referral process and implementation. Figure 2 illustrates the relationships between the barriers. Table 4 describes each sub-category, with a selected quote for each barrier.

Summary of barriers in health information systems and technologies to support maternal and neonatal referrals at PHCs
1) Technology
Due to the lack of IS/IT simplicity, the process of selecting hospitals is complicated for health workers. They can only refer patients to one hospital and must wait for a response before they make another referral. Delays in referral delivery and responses through this system make it difficult for health workers to refer patients quickly. Furthermore, the call center-based application (SPGDT) that is used nationally has a lack of availability during peak hours.
Existing applications cannot facilitate comprehensive referrals. One application can only serve one type of patient or referral. Another problem is the duplication of data work. For example, a health worker uses SIMPUS to record patient data during registration. When the patient needs to be referred, the health worker must re-enter the patient’s data in SISRUTE. Moreover, all respondents reported poor internet connections. The internet is only provided by the Ministry of Communications and Information (Kominfo), and there is no backup Internet provider.
2) Human resources
Health workers are not fully ready to use IS/IT due to their lack of IT knowledge or skills. Some applications can also increase their workload due to the need to input an excessive amount of data. Another problem is the lack of human resources to manage IS/IT who can be available at any time, especially to handle emergency referrals that need an immediate response.
3) Organizational support
A lack of financial support is one of the reasons why South Tangerang no longer uses SijariEMAS. Financial support is needed to perform server maintenance and training for health workers. Furthermore, a respondent at the DHO suggested that the lack of user involvement with SijariEMAS in South Tangerang stemmed from the absence of policies to involve all relevant stakeholders in the maternal and neonatal referral system.
4) Referral process and implementation
As a result of the above-mentioned IS/IT problems, health workers prefer using other communication media to refer patients or guiding patients and accompanying them to the preferred referral facility. Another problem is “hospital touring,” because IS/IT cannot help health workers to see hospitals’ capacity and make direct referrals to hospitals capable of admitting the patient. After referral, the hospital can return the patient to the PHC to continue treatment. However, this process is still done manually with a paper-based form. Moreover, there is no dashboard in the existing applications to see referral trends, such as the most referred health facilities and diseases, resulting in a lack of referral monitoring in this area.
III. Discussion
Functioning and available communication media make a significant contribution to referrals [22,23]. Applications that manage emergency cases should have a simple design even for non-computer-literate users [24]. IS/IT design should also facilitate referral comprehensively and consider all the characteristics of referrals [11]. In Indonesia, application developers often neglect existing IS/IT, which causes a lack of integration [25]. Enterprise architecture [14] and application programming interfaces [25] can serve as solutions to design integrated IS/IT. We proposed an architectural design for integrated health referral IS/IT in PHCs (Figure 3). To overcome internet problems, IS/IT should have the ability to work online and offline, with appropriate syncing [7,8]. The mobile internet, which offers more reliable connectivity, can also be considered [8].
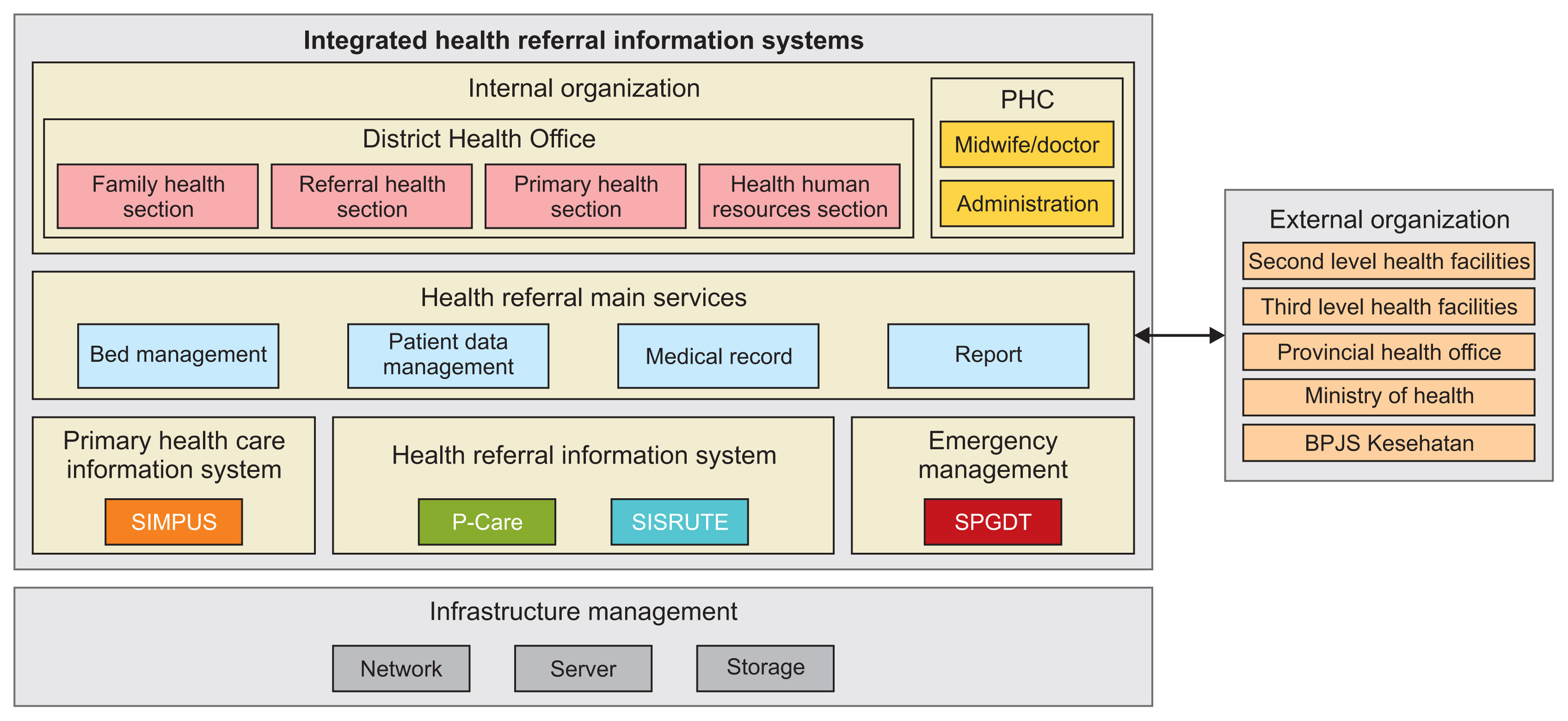
Architectural design of integrated health referral information systems. PHC: primary health centers, SIMPUS: Primary Health Care Information System, SISRUTE: Integrated Referral Information System, SPGDT: Integrated Emergency Management System, BPJS Kesehatan: Social Health Insurance Administration Body.
Human resources problems could be caused by the lack of health workers’ involvement in IS/IT development, which causes the technical requirements not to match their needs [25]. Training of human resources at all levels should be considered when implementing IS/IT [26]. Moreover, regulations in Indonesia should support IT personnel’s needs at PHCs [18]. Appropriate regulations are also needed to strengthen information flow across institutions [8]. Appropriate financial investment levels for IS/IT implementation should also be determined to ensure continuity [26].
This study contributes knowledge about IS/IT implementation in maternal and neonatal referral systems and provides recommendations for health regulators and application developers to implement IS/IT in Indonesia. Applications must consider the needs and capabilities of health workers and the infrastructure conditions. IS/IT policies should include all technological and social aspects and provide sufficient investments to ensure IS/IT continuity. As a limitation, the sample size of this study was small and it only focused on South Tangerang. Therefore, the results may apply only to this local area and not be generalizable to other settings. Future research should analyze IS/IT barriers from different perspectives and explore how IS/IT influences mothers’ and their families’ acceptance of referrals.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Acknowledgments
This work is a part of a master’s degree thesis of Nabila Clydea Harahap, Faculty of Computer Science, University of Indonesia.
We certify that this work is supported by Pendidikan Magister Menuju Doktor untuk Sarjana Unggul (PMDSU) grant Ministry of Research, Technology, and Higher Education (Contract No. NKB-3031/UN2.R3.1.HKP.05.00/2019).
The participant selection was conducted based on the letter of permission from the South Tangerang District Health Office (No. 070/1304/SDMK and 070/2206/SDMK).