|
 |
- Search
| Healthc Inform Res > Volume 27(4); 2021 > Article |
|
Abstract
Objectives
Health systems are shifting from traditional methods of healthcare delivery to delivery using digital applications. This change was introduced at a primary care centre in Chandigarh, India that served a marginalised population. After establishing the digital health system, we explored stakeholders’ perceptions regarding its implementation.
Methods
Ethnographic methods were used to explore stakeholders’ perceptions regarding the implementation of the Integrated Health Information System for Primary Health Care (IHIS4PHC), which was developed as a patient-centric digital health application. Data were collected using focus group discussions and in-depth interviews. Participatory observations were made of day-to-day activities including outpatient visits, outreach field visits, and methods of health practice. The collected information was analysed using thematic coding.
Results
Healthcare workers highlighted that working with the digital health system was initially arduous, but they later realised its usefulness, as the digital system made it easier to search records and generate reports, rapidly providing evidence to make decisions. Auxiliary nurse midwives reported that recording information on computers saved time when generating reports; however, systematic and mandatory data entry made recording tedious. Staff were apprehensive about the use of computer-based data for monitoring their work performance. Patients appreciated that their previous records were now available on the computer for easy retrieval.
Conclusions
The usefulness of the digital health application was appreciated by various primary healthcare stakeholders. Barriers persisted due to perceived needs for flexibility in delivering healthcare services, and apprehensions continued because of increased transparency, accountability, and dependence on computers and digital technicians.
Health systems are witnessing a transition from traditional methods of healthcare delivery to delivery with the aid of digital systems (also called eHealth systems). Digital systems are expected to improve the quality of care and doctor-patient communication to support patient-centred healthcare [1]. A key characteristic of patient-centred healthcare is the active involvement of patients in the care delivery process, which also involves a transition from hospital-based to community-based services [1–3].
However, despite technological advancements, the introduction of eHealth systems in primary healthcare (PHC) has been slow due to difficulties in embedding these systems in traditional healthcare delivery routines at the primary level. In India, many digital systems now support health programs [4]. However, poor internet connectivity, irregular electricity, problems with the design of the software programmes or the electronic devices themselves, and difficulties in understanding and using digital health technologies among healthcare workers (HCWs) plague the implementation of such systems [5–7].
The implementation of digital systems often has far-reaching implications extending beyond healthcare delivery. These include organizational, legal, operational, psychological, and social impacts [8]. Hence a significant resistance to adoption comes from HCWs. It is believed that the use of information technology (IT) by physicians has the potential to improve the quality of care in rural and underserved settings. However, some physicians feel that IT use hinders patient-doctor interactions [9] and increases apprehensions among healthcare providers. Physicians have been sceptical regarding the possibility of system breakdown and data loss [10]. Some professional values and personal feelings could also be barriers to eHealth interventions, as they may come into conflict with the use of technology. It has been argued that eHealth interventions should be adapted to fit pre-established work-flows for them to succeed [11]. However, most healthcare providers also perceive the usefulness of IT. The strong impact of IT is in turn influenced by its perceived ease of use, which is defined as “the degree to which a person believes that using a particular system would be free of effort” [12,13]. Regarding patient engagement, three dimensions can be impacted by eHealth interventions: behavioural (what a patient does, such as adhering to treatment), cognitive (what a patient thinks and knows, such as the consequences of disease), and emotional (what a patient feels, such as adjusting to changed life conditions due to a disease) [8].
Keeping the above-mentioned perspectives in mind, a patient-centric eHealth application, referred to as the Integrated Health Information System for Primary Health Care (IHIS4PHC), was tailored to address PHC needs in India [15]. It was developed using two open-source applications (openMRS and DHIS2). These applications have the functionalities of an Electronic Health Record, e-prescriptions, longitudinal tracking of clients, appointment reminders, targeted health education using SMS, and recording delivery for various health services (e.g., family planning advice or nutritional advice) delivered in the clinic as well as in community outreach. The IHIS4PHC digitised health delivery at multiple levels (i.e., individual, interpersonal, and organisational). It involved several components that interacted with each other to affect health outcomes. Evaluating the impact of this type of eHealth system is also a daunting task [14].
The efficacy of health interventions is usually evaluated through randomized controlled trials. However, there is no clear consensus on the most appropriate method to evaluate eHealth systems, which are considered to be highly complex [15]. In the realistic evaluation approach, rather than focusing solely on the question of “does it work?”, evaluators have been advised to also identify what works, in which circumstances, for whom, and why [16]. A mixture of quantitative and qualitative methods is often used to evaluate complex health interventions. Therefore, this qualitative study was conducted to assess the perceptions of various stakeholders about the implementation of IHIS4PHC in order to propose a model of behaviour change for eHealth using the theory of interpersonal behaviour (TIB) [17] and the capability, opportunity, and motivation from behaviour (COM-B) change wheel [18].
A qualitative approach was used to understand the processes related to the implementation of IHIS4PHC at a primary care centre in Chandigarh, India, during 2017 to 2018. This centre served approximately 25,000 individuals in urban slum populations, and it was staffed by three community physicians (CPs), three auxiliary nurse midwives (ANMs), two multipurpose workers (MPWs), and one sanitary attendant (SA). The study was approved by the Institutional Ethics Committee of the Postgraduate Institute of Medical Education and Research, Chandigarh, India (5370 dated 21/09/2016).
The IHIS4PHC was made fully functional in November 2017 after 11 months of research and development through a team of one public health researcher, one software developer, and one technical assistant. This team worked full-time with the staff of the primary care centre to understand the technical requirements. The Health Information System Programme (India) provided technical assistance for creating IT infrastructure and installation of the software. Several features were added to the system, such as graphical tracking of patients’ parameters (e.g., blood pressure and random blood glucose measurements) from previous clinic visits, generation of a fortnightly work plan for ANMs for scheduled services such as antenatal care (ANC), postnatal care (PNC), and immunizations, and automated SMS functionality for appointment reminders and health education. Household data were recorded in a “Family Folder,” which linked common household data to each household member and also captured household member relationships such as mother and child, husband and wife, and other similar relations with the head of the household. Depending on their health issues, household members were linked to various health modules such as ANC, PNC, immunization, non-communicable diseases, tuberculosis, and outpatient department (OPD) electronic health records [14]. Every time a module or functionality was added to the system, it was explained to the primary health centre staff. On-the-job training was provided to staff along with hands-on assistance while they worked on the system. A junior software developer and technical assistant provided on-the-spot support for any issues related to the eHealth system faced by the staff.
Qualitative research was undertaken after 6 months of full implementation of the IHIS4PHC. The qualitative assessment was done using in-depth interviews (IDIs) and focus group discussions (FGDs) by an independent investigator who had a background in the social sciences and expertise in conducting qualitative research. Participatory observation was undertaken by a public health researcher who worked with the staff from inception to full implementation of the eHealth system.
The IHIS4PHC implementation was aimed to make the health system more efficient to improve the overall experiences of healthcare providers and clients. Therefore, the views of both healthcare staff and clients/patients were assessed. Users’ perspectives regarding IHIS4PHC were appraised using IDIs with six purposively selected key informants (three CPs, two ANMs, and one MPW) from the primary care centre and three FGDs with randomly selected clients who had utilized any kind of services at the primary care facility where IHIS4PHC was implemented.
To assess the patient-centredness of the eHealth system, FGDs were held with the clients. Each FGD had six to eight participants. Out of the three FGD groups, the first group was a mixed group comprising both men and women, the second group comprised men only, and the third group had only women. Since most of the population belonged to lower socio-economic groups and the possibility of bias due to gender-related hesitancy was raised during discussions, FGDs with different compositions were conducted in order to elicit independent views from clients of both genders, while one mixed group was added to focus on their common views. A participant information sheet and a topic guide for the IDIs and FGDs were prepared with consultation with experts. The IDIs and FGDs were audio-recorded after obtaining permission from the participants. The IDIs and FGDs lasted for about 60 minutes.
In the participatory observations, the researcher recorded how healthcare providers carried out their work at the primary care centre. The researcher with expertise in public health was involved with the staff at the primary care centre to identify the needs of the staff and clients/patients, to provide input for the development of IHIS4PHC and to carry out quality checks. The researcher also made observations of day-to-day activities such as OPD work, outreach field visits, and the health practice methods used, and also carried out unstructured interviews with healthcare providers on their views of the eHealth system as a facilitator or barrier to their work. The researchers recorded descriptive (settings, actions, behaviours, conversations) and reflective (thoughts, ideas, questions, and concerns during observation) information in field notes.
Qualitative data were analysed using the thematic analysis technique. The codes used were emergent codes—that is, codes that emerged from the data using the grounded theory approach [19].
In total, 20 adults (12 women and 8 men) participated in the three FGDs. The mean age of the participants was 48 years (range, 19–64 years). The majority of the participants had education up to the senior secondary level, two were graduates, and four were illiterate (all women). Thirteen of them had hypertension or diabetes, three were receiving ANC or PNC, and four of them had visited the health facility for an acute illness. The FGDs with clients were focused on an assessment of the impact of the eHealth system on the health services provided to them. In contrast, the IDIs with HCWs were concerned with their experiences of working with the eHealth system. These HCWs included the three CPs who managed the clinic, one MPW who managed the drug inventory, registration of patients, and drug dispensing, and two ANMs who provided reproductive and child healthcare services. The participatory observations conducted by a public health researcher used a pragmatic approach for process analysis of the implementation of the eHealth intervention. Important themes that emerged from the IDIs, FGDs, and participatory observations are presented below.
Working with an IT-enabled health system was arduous initially. For example, a doctor mentioned:
“it is cumbersome to select separately from drop-down menus for a medicine’s name, composition, dose, and frequency.” (IDI-1, CP)
The consultation time increased by about 2 minutes per patient as the doctor had to make entries in the computer by himself or herself.
The habitual way of working with a paper-based system and issues related to inflexibility and complexity in the computer-based system acted as deterrents to the adoption of the eHealth system by HCWs. They found the data entry forms in the computer to be lengthier, as now they had to enter a comprehensive range of mandatory socio-demographic details that could be left blank in the paper-based system. The ANMs still had to work with a paper-based system, as the state administration insisted on maintenance of registers and preparation of paper-based reports, also which resulted in two parallel systems; thus, the gains expected from the eHealth system could not be fully realized.
The HCWs later recognized the usefulness of IT after using it for some time, because they could easily search patients’ records, generate reports, and look for evidence to make decisions. Moreover, with its prompts, the IT platform offered comprehensive, integrated care combining preventive, promotive, and curative care. It saved time spent on entering the same information in multiple registers and in multiple reports, which used to take more than 50% of their work time that could now be used for patient care (Tables 1, 2).
The inventory for dispensing and maintaining medicines in the computer system was very helpful, as expressed by para-medical staff:
The eHealth system resolved many of the stock maintenance-related issues, such as real-time maintenance of the stock balance, and provided timely alerts of depleted medicine stores. In order to improve work efficiency and to reduce errors, it was considered important that real-time direct entries were made to fully shift to the computer system (Table 3).
However, it was observed that low competency in handling the eHealth tools acted as a barrier to the full implementation of the eHealth system. Healthcare providers had to depend on the technical assistant for even minor trouble-shooting tasks.
The absence of clear directions from the government and the likelihood that the government will launch new electronic applications posed a dilemma for the healthcare providers regarding the full adoption of the eHealth intervention (Table 4).
Integrated healthcare requires teamwork to produce quality results. If any of the team members are not fully convinced to use the eHealth system, then it may defeat the purpose of integrated care, as can be deduced from the following statement:
“The registration person doesn’t put in the effort to search for a patient in the system and re-registers the patient, so sometimes patient tracking gets difficult due to multiple entries for the same patient.” (IDI-3, ANM)
An integrated system reduced duplication of work. However, it was considered to be more complex. Errors, if any, were reflected in the entire eHealth system, which was not a problem in the fragmented paper-based system. In the paper-based system HCWs could do multiple tasks independently and whenever additional tasks were added by administration, they could prioritise the essential tasks required for reporting (Table 4). The flexibility in the computer system was limited, meaning that the healthcare providers needed to follow a systematic approach for adopting the integrated eHealth system.
One of the main issues that emerged from IDIs with HCWs was that the maintenance of the eHealth system requires on-the-spot technical support to ensure uninterrupted work, especially in the OPD as sometimes the computer may “hang” or paper may “jam” in the printer. Issues related to the handling of IT equipment, uninterrupted electrical supply, and fears of a computer system breakdown were major concerns (Table 3).
However, computerization made PHC more systematic and responsive. During FGDs with clients, it was revealed that the health facility is now more organized, with improved services, reduced waiting time, and greater medicine availability. At every clinic visit, patients’ height, weight, blood pressure, and blood sugar were checked and clients were informed of their status from the previous visit. Clients were happy to receive appointment reminder messages and health promotion messages through SMS, which prompted them to take medicines on time, reduce salt intake, improve their diet, and take other steps to promote their health (Table 5).
The increased transparency with the implementation of the integrated eHealth system made healthcare providers somewhat insecure. The eHealth system increased their work stress as healthcare providers had to improve their competency to operate computers and be more careful with data entry, as they had to maintain constant vigilance regarding administrators (Table 4).
HCWs were apprehensive about the enhanced ease of monitoring by the primary care centre in-charge through the eHealth system, as they were being questioned more frequently regarding the correction of errors, which was perceived as “surveillance” by the staff; for this reason, they resisted adoption of the eHealth system (Table 1).
The clients did not feel the computer system to be a hindrance to doctor-patient communication. They felt that doctors’ tasks had increased, as doctors now had to spend more time in the consultations. They stated:
“We do feel that the doctors keep looking at the computer, but they are able to make quick entries.” (FGD-1, mixed group)
They felt that the doctors now asked fewer questions than before, which may have been because their basic information was already recorded in the computer system. Clients expressed their satisfaction with computerized registration and electronic prescriptions, which they felt made the process systematic and more efficient, with reduced errors (Table 5).
Clients stated that the registration process had become fast. They were no longer asked about their previous prescription slips, as their previous health records were available for multiple doctors on the computer. The e-prescription had more complete information. One participant stated:
“The doctor forgot to inform me about my high sugar level, which was recorded on the e-prescription, but later it was observed by another doctor when he checked my e-prescription slip.” (FGD-2, women)
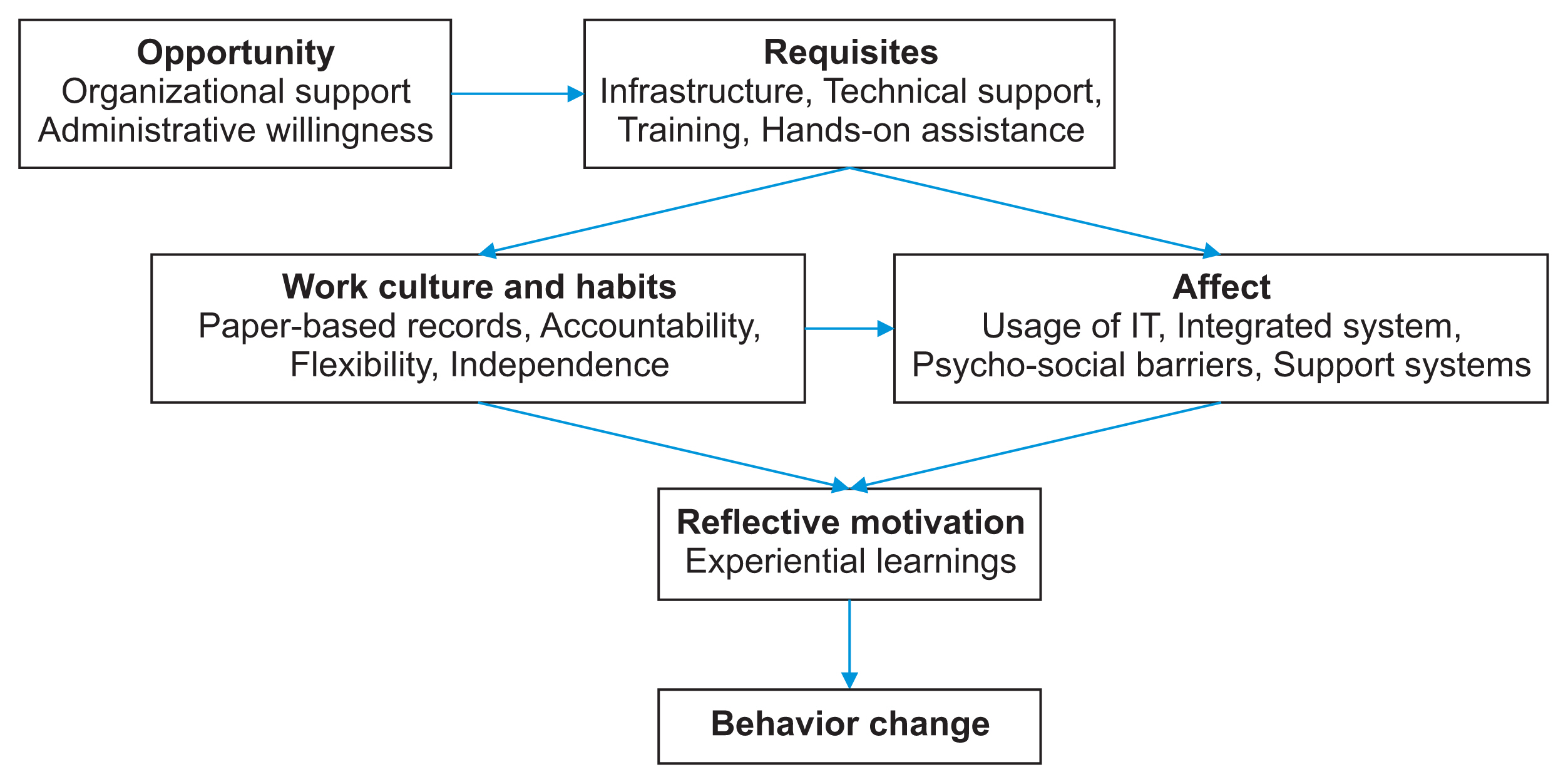
The above findings were further categorised using the TIB and COM-B models. The interconnections between these categories are presented in Figure 1 to explain the behaviour change related to the eHealth intervention.
Qualitative methods were used to understand the psycho-social and technical factors affecting the implementation of IHIS4PHC in a primary care centre using the constructs of TIB [17] and COM-B model [18]. The qualitative approach facilitated appreciation of the issues faced by HCWs while they worked with the eHealth system, as well as the perceptions of clients/patients regarding the impact of the eHealth system on the healthcare services delivered to them.
All HCWs expressed that the eHealth system improved the quality of data—that is, it reduced duplication, errors were minimized, and report generation became very efficient with high reliability. In most other settings, eHealth systems have likewise improved efficiency, communication, and the accessibility and accuracy of data [10,14,20]. The present study captured the issues faced by both clients and HCWs during the introduction and maintenance of the eHealth system in a primary care centre serving a vulnerable population where clients had low literacy.
Initially, the HCWs complained that it took additional time to make entries in the computer, and it was a cumbersome process. They reported a number of technical issues, such as breakdowns of hardware, bugs in the software, and an erratic electricity supply. They felt that the eHealth system did not provide the flexibility that a paper system could, as in many places drop-down menus restricted the selection of options. As in other studies, these were considered barriers to the smooth day-to-day functioning of the primary care centre [11]. HCWs were also quite apprehensive that they might become dependent on the eHealth system.
An important benefit recognised by the HCWs was the feasibility and convenience of longitudinal follow-up of chronic patients, which was not possible with the paper-based system [21]. They appreciated that at a later stage it might be easier to extract data or generate reports from computerized records, which would save time.
The eHealth system did not allow flexibility in the form of short-cuts. Making the workflow transparent led to an increase in responsibility, as the system made people more accountable. The ease of monitoring and requirements in terms of competency and skills to operate eHealth system were reasons for poor responses by eHealth system healthcare providers.
In addition to facilitating the functioning of healthcare providers, the patient-centric eHealth system IHIS4PHC also aimed to improve the healthcare provided to the clients/patients. The eHealth system did not seem to hinder community health services and patient care. Instead, the clients/patients found it to be beneficial. The system helped in efforts to reach out to the clients/patients, provided health information specific to their health conditions, improved medicine supplies, ensured longitudinal care, and systematized the functioning of the primary care centre, thereby building the confidence of clients/patients in PHC.
The clients assessed the impact of the eHealth intervention impact on the function of the primary care facility, which provided insights into their outlook on the eHealth system. The clients shared that computers in the primary care facility enabled systematic functioning (e.g., registration, triage and consultation, better time management, complete check-ups, and printed prescriptions) and ensured medicine availability for a month for chronic illnesses, all of which made the health services more user-friendly. Clients from India and other countries have shared similar experiences with eHealth systems [10,22,23].
Although the implementation of the eHealth system in primary care was technically feasible, its acceptance and use by healthcare providers and service users were low in the initial phases of the intervention. There were “teething” problems in the beginning, but continuous psycho-social support and hands-on assistance changed the perceptions. Both service users and providers eventually appreciated the advantages of the eHealth system.
Since the eHealth system is client-friendly and improved service delivery, it is important to establish the links between factors that led to behaviour change despite resistance due to perceived problems. The TIB and COM-B were applied to propose a model to present how the eHealth intervention led to behaviour change. While the TIB has often been used for internet use at the workplace to explain that how cognition, affect, and habits bring about change, the COM-B model states that opportunity and motivation are equally important, along with the capability for behaviour change, especially for service providers in health systems. The proposed model (Figure 1) depicts how opportunities led to requisites, requisites led to changes in work culture and perceptions, then these two together influenced the motivational level (i.e., reflective motivation) through experiential learning, which ultimately led to behaviour change.
In conclusion, the development and implementation of eHealth systems at any level constitute a complex intervention. An appraisal of an eHealth system by the stakeholders helps to understand the complexities and how to navigate through these complexities to convert interventions into sustainable programs. This study has outlined the factors that need to be considered for behaviour change, the barriers that can be encountered in the early stages, and the efforts needed to implement an eHealth intervention within the imperfect health systems of most low-and middle-income countries. It is equally important to note that the vulnerable populations also accepted the usage of the eHealth system and appreciated the improvements to the quality of services. The eHealth system definitely helped to reach the unreached population. Further evidence and lessons from other contexts will also be useful. Policymakers should consider eHealth systems as a strategy for improving the quality of the health system.
Acknowledgments
We are thankful to Norwegian Research Council for funding of the research work and University of Oslo, Norway & HISP, India for providing the technical help. We are also grateful to Mr Dilroop, and Mr Akash, who helped us with the customization and functionalities development in the IHIS4PHC software as per the needs of health care providers. We are extremely obliged to the staff of Primary Health Centre at sector-25, Chandigarh and participants of focused group discussion from the community who agreed to participate in the study and share their views.
Table 1
Community physicians’ perceptions of the eHealth system
Table 2
Auxiliary nurse midwives’ perceptions of the eHealth system
Table 3
Multipurpose worker’s perceptions of the eHealth system
Table 4
Public health researcher’s participatory observations on the eHealth system
Table 5
Clients’ perceptions of the eHealth system
References
1. Flatley Brennan P, Kuang YS, Volrathongchai K. Patient-centered Information Systems. Yearb Med Inform 2000;(1):79-86.


2. Kotze P, Foster R. A conceptual data model for a primary health care patient-centric electronic medical record system [Internet]. Calgary, Canada: ACTA Press; 2014 [cited at 2021 Sep 30]. Available from: https://doi.org/10.2316/p.2014.815-010

3. Berwick DM. What ‘patient-centered’ should mean: confessions of an extremist. Health Aff (Millwood) 2009;28(4):w555-65.


4. Faujdar DS, Sahay S, Singh T, Jindal H, Kumar R. Public health information systems for primary health care in India: a situational analysis study. J Family Med Prim Care 2019;8(11):3640-6.



5. Tripathi S, Sharma R, Nagarajan S. Health information systems in India: challenges and way forward [Internet]. Munich, Germany: Munich Personal RePEc Archive (MPRA); 2018 [cited at 2021 Sep 30]. Available from: https://mpra.ub.uni-muenchen.de/87067/

6. Ndabarora E, Chipps JA, Uys L. Systematic review of health data quality management and best practices at community and district levels in LMIC. Inf Dev 2014;30(2):103-20.

7. Singh T, Roy P, Jamir L, Gupta S, Kaur N, Jain DK, et al. Assessment of universal healthcare coverage in a district of North India: a rapid cross-sectional survey using tablet computers. PLoS One 2016;11(6):e0157831.



8. Barello S, Triberti S, Graffigna G, Libreri C, Serino S, Hibbard J, et al. eHealth for patient engagement: a systematic review. Front Psychol 2016;6:2013.



9. Sequist TD, Cullen T, Hays H, Taualii MM, Simon SR, Bates DW. Implementation and use of an electronic health record within the Indian Health Service. J Am Med Inform Assoc 2007;14(2):191-7.



10. Mannan R, Murphy J, Jones M. Is primary care ready to embrace e-health? A qualitative study of staff in a London primary care trust. Inform Prim Care 2006;14(2):121-31.


11. Granja C, Janssen W, Johansen MA. Factors determining the success and failure of eHealth interventions: systematic review of the literature. J Med Internet Res 2018;20(5):e10235.



12. Li J, Talaei-Khoei A, Seale H, Ray P, Macintyre CR. Health care provider adoption of eHealth: systematic literature review. Interact J Med Res 2013;2(1):e7.



13. Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q 2003;27(3):425-78.

14. Faujdar DS, Sahay S, Singh T, Kaur M, Kumar R. Field testing of a digital health information system for primary health care: a quasi-experimental study from India. Int J Med Inform 2020;141:104235.


15. Lilford RJ, Foster J, Pringle M. Evaluating eHealth: how to make evaluation more methodologically robust. PLoS Med 2009;6(11):e1000186.



16. Pawson R, Tilley N. Realist evaluation [Internet]. London, UK: Sage; 2004 [cited at 2021 Sep 30]. Available from: http://www.communitymatters.com.au/RE_chapter.pdf

17. Gagnon MP, Legare F, Fortin JP, Lamothe L, Labrecque M, Duplantie J. An integrated strategy of knowledge application for optimal e-health implementation: a multi-method study protocol. BMC Med Inform Decis Mak 2008;8:17.



18. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42.



19. Foley G, Timonen V. Using grounded theory method to capture and analyze health care experiences. Health Serv Res 2015;50(4):1195-210.


20. Adane K, Muluye D, Abebe M. Processing medical data: a systematic review. Arch Public Health 2013;71(1):27.



21. Talboom-Kamp EP, Verdijk NA, Harmans LM, Numans ME, Chavannes NH. An eHealth platform to manage chronic disease in primary care: an innovative approach. Interact J Med Res 2016;5(1):e5.



- TOOLS