1. Hanoum IF, Boediono A, Pangestu M, Haryadi D, Widad S, Dasuki D. Microvolume of 0.1 ╬╝L gama sleeved cryoloops for blastocyst vitrification of assisted reproductive technology patients. Jurnal Kesehatan Reproduksi 2015 2(1):47-52.
https://doi.org/10.22146/jkr.7127

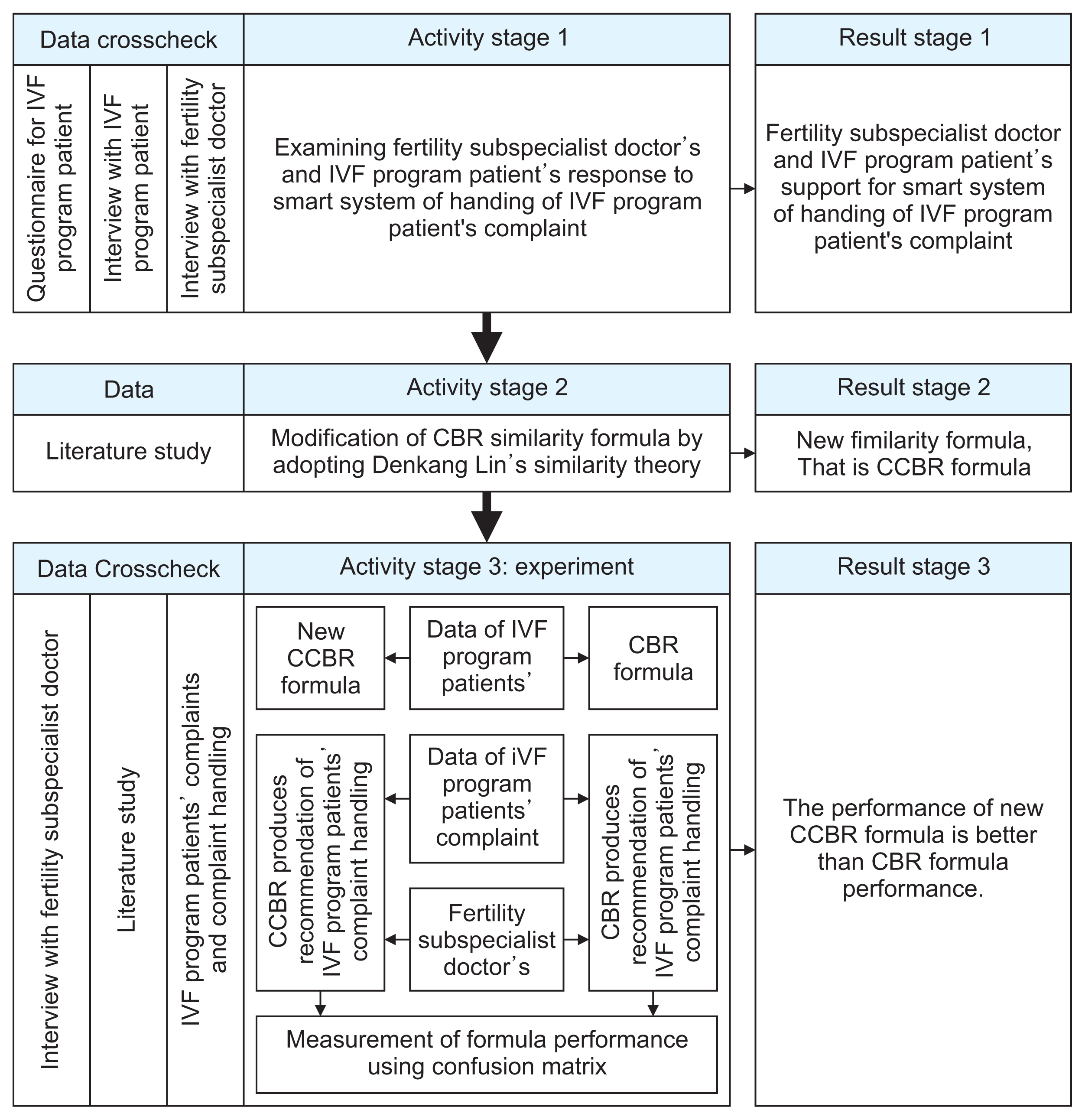
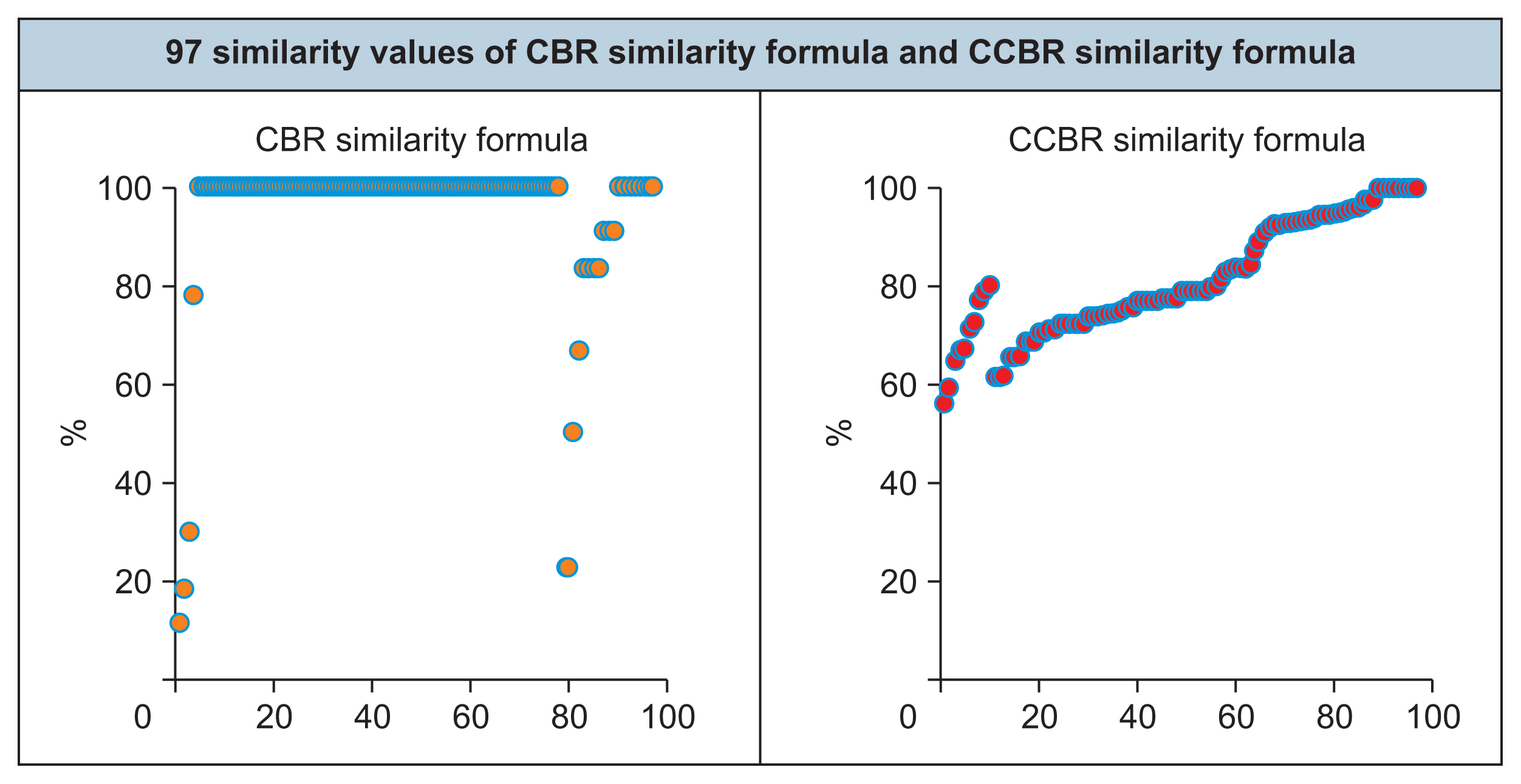
2. Christianto PA, Sediyono E, Sembiring I. Case-based reasoning modifications for intelligent systems in handling in vitro fertilization (IVF) patients post embryo transfer. Proceedings of 2020 International Seminar on Application for Technology of Information and Communication (iSemantic); 2020 Sep 19ŌĆō20. Semarang, Indonesia; p. 109-14.
https://doi.org/10.1109/iSemantic50169.2020.9234270

3. Christianto PA, Sediyono E, Sembiring I, Wijono S. editors. Intelligent system of handling in vitro fertilization (IVF) patients post embryo transfer to reduce the level of patient anxiety and help fertility doctors quickly answer patient questions. In: In : Triwiyanto , Nugroho HA, Rizal A, Caesarendra W, Proceedings of the 1st International Conference on Electronics, Biomedical Engineering, and Health Informatics; Singapore: Springer; 2021. p. 183-96.
https://doi.org/10.1007/978-981-33-6926-9_17

4. Bennett L, Pangestu M. Regional reproductive quests: cross-border reproductive travel among infertile Indonesian couples. Asia Pac Viewp 2017 58(2):162-74.
https://doi.org/10.1111/apv.12160

5. Guven PG, Cayir Y, Borekci B. Effectiveness of acupuncture on pregnancy success rates for women undergoing in vitro fertilization: a randomized controlled trial. Taiwan J Obstet Gynecol 2020 59(2):282-6.
https://doi.org/10.1016/j.tjog.2020.01.018


6. Capuzzi E, Caldiroli A, Ciscato V, Zanvit FG, Bollati V, Barkin JL, et al. Is in vitro fertilization (IVF) associated with perinatal affective disorders? J Affect Disord 2020 277:271-8.
https://doi.org/10.1016/j.jad.2020.08.006


9. Chen S, Guo X, Wu T, Ju X. Exploring the online doctor-patient interaction on patient satisfaction based on text mining and empirical analysis. Inf Process Manag 2020 57(5):102253.
https://doi.org/10.1016/j.ipm.2020.102253

11. Gozuyesil E, Karacay Yikar S, Nazik E. An analysis of the anxiety and hopelessness levels of women during IVFET treatment. Perspect Psychiatr Care 2020 56(2):338-46.
https://doi.org/10.1111/ppc.12436


15. Bras de Guimaraes B, Martins L, Metello JL, Ferreira FL, Ferreira P, Fonseca JM. Application of artificial intelligence algorithms to estimate the success rate in medically assisted procreation. Reprod Med 2020 1(3):181-94.
https://doi.org/10.3390/reprodmed1030014

16. Song K, De Jonckheere J, Zeng X, Koehl L, Yuan X, Zhao X. Development of a data-based interactive medical expert system for supporting pregnancy consultations: general architecture and methodology. IFAC-PapersOnLine 2019 52(19):67-72.
https://doi.org/10.1016/j.ifacol.2019.12.109

18. Gou X, Xu Z, Wang X, Liao H. Managing consensus reaching process with self-confident double hierarchy linguistic preference relations in group decision making. Fuzzy Optim Decis Mak 2021 20(1):51-79.
https://doi.org/10.1007/s10700-020-09331-y

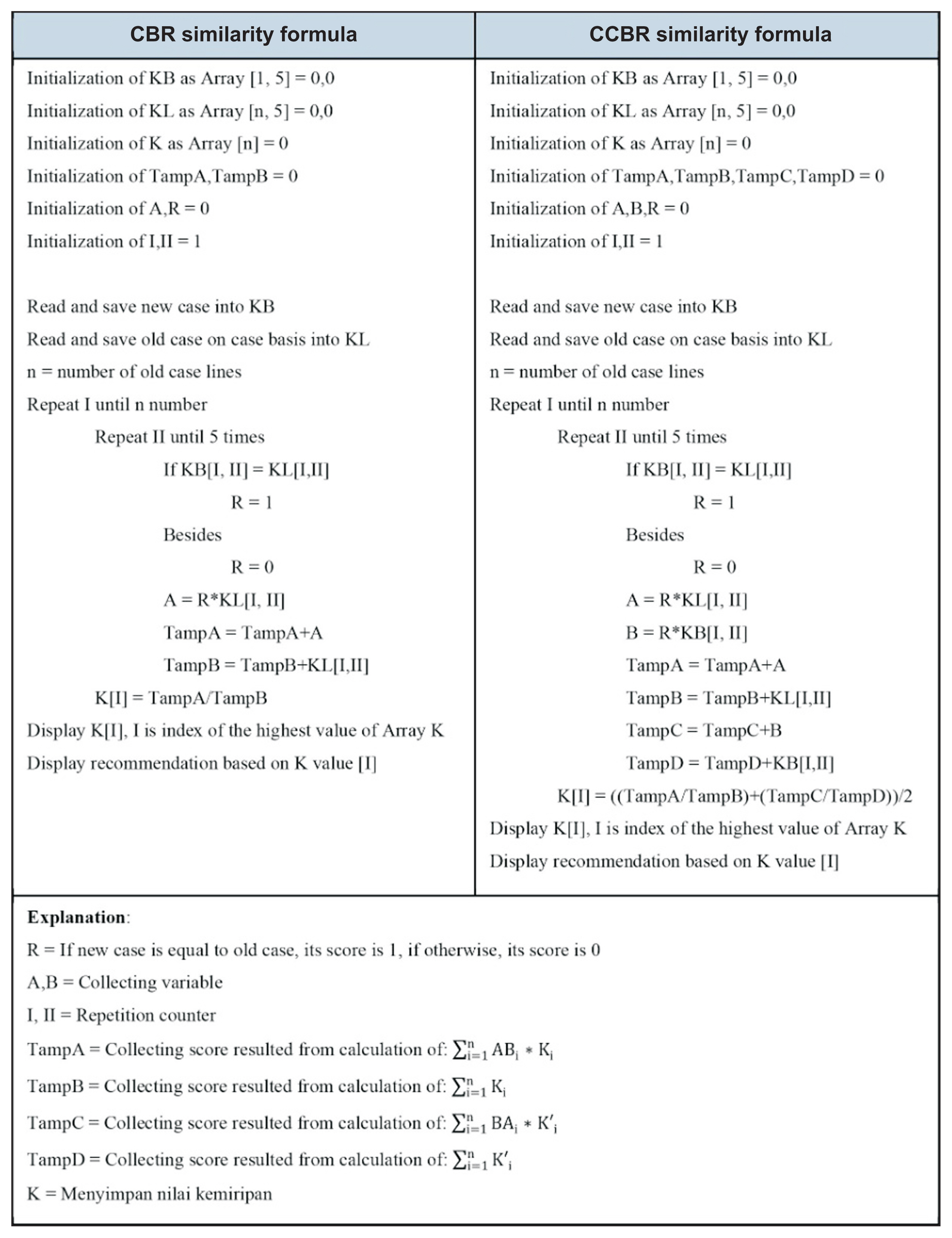
22. Lin D. An information-theoretic definition of similarity. Proceedings of the 15h International Conference on Machine Learning (ICML); 1998 Jul 24ŌĆō27. Madison, WI; p. 296-304.

23. Bentaiba-Lagrid MB, Bouzar-Benlabiod L, Rubin SH, Bouabana-Tebibel T, Hanini MR. A case-based reasoning system for supervised classification problems in the medical field. Expert Syst Appl 2020 150:113335.
https://doi.org/10.1016/j.eswa.2020.113335

26. Adeniyi DA, Wei Z, Yang Y. Risk factors analysis and death prediction in some life-threatening ailments using chi-square case-based reasoning (Žć
2 CBR) Model. Interdiscip Sci 2018 10(4):854-74.
https://doi.org/10.1007/s12539-018-0283-6