Development of a Nursing Practice Guideline for Pre and Post-Operative Care of Gastric Cancer Patients
Article information
Abstract
Objectives
The aim of this study was to develop nursing practice guidelines and algorithms for the pre- and postoperative care of gastric cancer patients.
Methods
The guidelines and algorithms were developed based on a literature review and subject-matter experts' knowledge. The usefulness and applicability of the developed guidelines and algorithms were evaluated by the expert group.
Results
The guidelines comprised 64 recommendations and algorithms for admission care, preoperative care on the day before the operation, preoperative care on the operation day, immediate postoperative assessment, postoperative care, and discharge care of gastric cancer patients. After appropriate evaluation, the experts declared the guidelines to be both useful and applicable.
Conclusions
The guidelines developed in this study can be used for patient care and for training nursing students and novice nurses. In addition, these guidelines can be integrated into the electronic nursing record system for clinical decision support in the future. This will improve the quality of clinical nursing and the expertise of nurses.
I. Introduction
There is currently a tendency to shorten the length of hospital stay, with patients being discharged early to reduce medical costs and to increase the turnover rate of beds in the healthcare sector. Thus, healthcare professionals need to provide patients with the most effective and intensive care during relatively short stays in hospital. This has increased the introduction of clinical decision support system (CDSS) to assist clinical practitioners in their decision-making regarding the most appropriate healthcare for specific clinical circumstances. Most existing technology of the CDSS uses clinical practice guidelines as the support base [1]. Clinical practice guidelines provide healthcare professionals with knowledge and information drawn from the systematic review of research findings and expert knowledge of healthcare professionals. Healthcare professionals can thus ultimately make rational and integrated clinical decisions in practice using this knowledge and information [2,3]. According to a systematic review of 18 studies on the effect of nursing practice guidelines, the use of such guidelines was found to be effective in changing the process such as improving the accuracy of nursing records and outcome of nursing activities such as decreasing the incidence of complications [4]. In addition, clinical practice guidelines reduce inappropriate variations in practice, promote the quality of healthcare, and enable healthcare professionals to explain the rationale underlying their interventions [5,6].
The need for clinical guidelines is only just starting to be recognized in Korea, and culturally relevant clinical guidelines are now starting to be developed. A few studies have tested the applicability of clinical guidelines developed by international organizations that are widely used in other countries, and adapted for use in Korea, such as those for self-voiding promotion [7], acute pain management [8,9], and constipation management [10]. Several guidelines have recently been developed in Korea, such as those for the management of patients with acute confusion [11], care for patients with head injuries [12], constipation management for the elderly [13], and care for enteral feeding [14]. However, no guidelines have yet been developed to cover the nursing care for patients who are undergoing surgery.
The incidence rate of gastric cancer in Korea is the highest of all of the cancers, accounting for 18.3% of the major cancers [15]. Surgical removal is considered to be the most effective treatment for gastric cancer patients, even though there have been notable advances in cancer treatments [16]. Since surgical removal of the stomach of gastric cancer patients is the most frequent of the abdominal surgeries, it is important to develop nursing practice guidelines for the pre- and postoperative care of gastric cancer patients. It is also important for nurses to be able to detect and respond expeditiously to the possible postoperative complications of gastrectomy-such as hemorrhage, anastomosis-site leakage or obstruction, reflux gastritis, dumping syndrome, and malabsorption-by the monitoring and close observation of patients [17].
The Scottish Audit of Surgical Mortality highlighted problems in the perioperative management of surgery patients in its annual report, particularly emphasizing variations in practice in postoperative care [18]. It called for the development of best-practice guidelines for surgery patients, especially since 1,000 patients suffer from major complications following surgery annually in Scotland. Therefore, the Scottish Intercollegiate Guidelines Network (SIGN) developed guidelines for the management of symptoms and signs of major postoperative complications [18]. However, the target population of these guidelines is all surgery patients, including gastric surgeries; it was designed for use in all units, including high-dependency units and intensive care units, as well as general wards; and the target audience for the guidelines includes doctors, paramedical staff, and nurses. These guidelines are thus not sufficiently specific to be used in the surgical wards providing pre- and postoperative care for gastric cancer patients. Therefore, it was deemed necessary to develop nursing practice guidelines suitable for clinical practice in Korea and designed specifically to address the pre- and postoperative care of gastric cancer patients in a rapid and systematic way.
This study was therefore conducted to develop guidelines based on a literature review of the pre- and postoperative nursing care of gastric cancer patients. The nursing practice guidelines developed in this study will improve not only the quality of nursing care but also the expertise of nurses. They may also be used to educate nursing students and novice nurses in the pre- and postoperative nursing care of gastric cancer patients.
II. Methods
This was a methodological study designed to develop nursing practice guidelines for the pre- and postoperative nursing care of gastric cancer patients in two stages: 1) the guidelines were developed based on a literature review and experts' knowledge, and 2) the usefulness and applicability of the guidelines were evaluated by a group of nurse experts.
1. Development of the Nursing Practice Guidelines
1) Review of the literature on pre- and postoperative nursing care for gastric cancer patients
We reviewed and analyzed articles published in academic nursing journals and textbooks on nursing and medicine related to nursing care before and after surgery of gastric cancer patients. We classified nursing care before and after surgery into six categories: admission care, preoperative care for the day before the operation, preoperative care for the operation day, immediate postoperative assessment, postoperative care, and discharge care. Detailed care items for each category were retrieved. Postoperative care was further classified into six subcategories of care: preventive care for pulmonary complications, management of the surgical wound, management of drainage · foley catheter, management of pain, management of nutrition, and preventive care for venous thromboembolism, based on a care flow of nurses. Detailed care items for each subcategory were retrieved.
The literature was searched using keywords such as "nursing for abdominal surgery patients" and "nursing for gastric cancer patients" and then limited to articles with pre- and postoperative nursing care for gastric cancer patients. Further searches of the six subcategories of postoperative nursing care (preventive care for pulmonary complications, management of the surgical wound, management of drainage · foley catheter, management of pain, management of nutrition, and preventive care for venous thromboembolism) were also performed. We limited articles published between 1985 and 2008.
2) Development of nursing practice guidelines and algorithms for the pre- and postoperative nursing care of gastric cancer patients
Nursing care items were developed based on the literature review and arranged according to categories of pre- and postoperative nursing care practice of gastric cancer patients. These nursing care items were verified by nurses who have worked in general surgery units for more than 3 years. Nurses verified whether all of the nursing areas for surgery patients with gastric cancer were covered, whether the flow of the algorithm was appropriate, and whether the care items were expressed appropriately. Reflecting the opinions of the clinical nurse experts on the items, recommendations of the nursing practice guidelines were developed, as were algorithms displaying the flow of recommendations in the guidelines.
3) Validation test of the guidelines by nurse experts
The content validity of the developed guidelines was tested by the nurse expert group. Fourteen nurses who have worked in general survey units for more than 3 years participated in the content validity evaluation between October 14 and 21, 2008. A questionnaire utilizing a five-point Likert response scale ranging from "never appropriate" to "very appropriate" was used to rate the appropriateness of the content of each recommendation of the guidelines. An index of content validity (CVI) of each recommendation was computed and any recommendations with a CVI agreement of more than 80% were regarded as appropriate. If there were any recommendations with more than one comment regarding applicability in clinical practice, a secondary meeting involving a smaller group of experts (four head nurses in a general surgical ward) and two consultants was convened to determine whether the recommendation should be kept in the guidelines. Two consultants consisted of a surgeon who was a clinical professor with more than 6 years of working experience in general surgery and a gastric cancer care coordinator who was a nurse with more than 10 years of working experience in nursing and more than 5 years of working experience in gastric cancer care.
4) Confirmation of the final version of the nursing practice guidelines
Based on the content validation, the guidelines for the pre- and postoperative nursing care of gastric cancer patients was modified and finalized.
2. Evaluation of the Usefulness and Applicability of the Developed Guidelines
The usefulness and applicability of the guidelines were evaluated by 21 nurse experts, including 4 head nurses in general surgical units and 17 nurses who had been working in general surgical units for more than 1 year, using a questionnaire between November 3 and 14, 2008. The nurse experts were asked to rate the usefulness and applicability of the 64 recommendations in the guidelines using a five-point Likert rating scale ranging from "very low" to "very high."
III. Results
1. Development of the Nursing Practice Guidelines
1) Review of the literature on the pre- and postoperative nursing care of gastric cancer patients
In total, 54 articles were searched and used to generate recommendations for the nursing practice guidelines. However, since there were insufficient studies related to the postoperative nursing care of gastric cancer patients, most of the searched articles on this topic were used to develop the clinical practice guidelines.
2) Development of nursing practice guidelines for the pre- and postoperative nursing care of gastric cancer patients
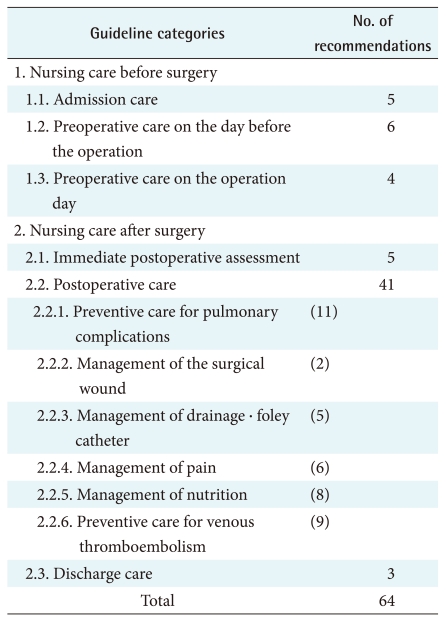
Nursing practice guidelines for the pre- and postoperative nursing care of gastric cancer patients comprised two domains of nursing care: before and after surgery. The nursing care before surgery includes admission care, preoperative care on the day before the operation, and preoperative care on the operation day (15 recommendations), while the nursing care after surgery includes immediate postoperative assessment, postoperative care, and discharge care (49 recommendations). The six subcategories of postoperative care constituted 41 recommendations. The hierarchical structure of the guidelines and the number of recommendations for each category are listed in Table 1.
3) Validity test of the guidelines
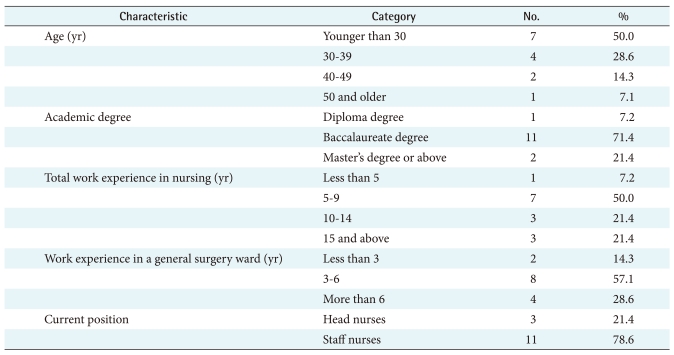
The nurse experts who participated in the evaluation of the content validity of the guidelines comprised 3 head nurses and 11 nurses with more than 3 years of experience working in a general surgical care unit. Nurses who aged 30 years or younger accounted for 50% of the group. With regard to work experience, 57% had worked in a general surgical care unit for 3-6 years and 50% had worked for a total of 5-9 years as a nurse (Table 2).
The nurse experts agreed that five of the six categories (the exception was postoperative care) were valid, with a CVI of more than 80%. In the subcategories of the postoperative care category, four recommendations, including management of drainage · foley catheter and preventive care for venous thromboembolism, had a CVI of less than 80%. Another meeting with four head nurses from general surgical care units, one surgeon, and one gastric cancer coordinator was convened to review these four recommendations. As a result, two of them were modified and kept, and the other two were removed from the guidelines, as presented in Table 3.
4) Final version of the nursing practice guidelines
The nursing practice guidelines for the pre- and postoperative care of gastric cancer patients and the associated algorithms were finalized after modification and deletion of some recommendations based on the findings of the content validity test. The guidelines' algorithms comprise two parts: nursing care before and after surgery. Three examples of algorithms developed for nursing practice guidelines are shown in Figures 1-3: Figure 1 shows the algorithm of nursing care before surgery with the flow of admission care, preoperative care on the day before the operation, and preoperative care on the operation day; Figure 2 shows the flow of immediate postoperative assessment, postoperative care, and discharge care as part of the nursing care after surgery; and Figure 3 shows the flow of preventive care for venous thromboembolism, as one of the six subcategories of postoperative care.

Algorithm for the nursing practice guidelines developed for nursing care before surgery in gastric cancer patients.
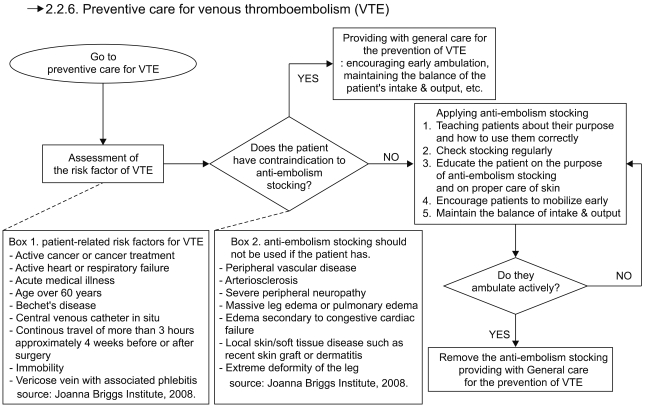
Algorithm for nursing practice guidelines developed for the preventive care for venous thromboembolism.
2. Evaluation of the Usefulness and Applicability of the Nursing Practice Guidelines
The usefulness and applicability of the guidelines were evaluated by 21 nurse experts in a general surgical care unit. The average usefulness and applicability scores of each category, as presented in Table 4, were 4.7 and 4.5 out of 5.0, respectively. The usefulness and the applicability scores of most of the recommendations exceeded 4.0; however, the recommendation for the management of pain had the lowest scores (4.3 for usefulness and 3.9 for applicability), followed by that for preventive care for venous thromboembolism (4.5 for usefulness and 4.3 for applicability). The remaining recommendations had scores of at least 4.5 for usefulness and applicability.
IV. Discussion
By reviewing articles in nursing journals and textbooks of nursing and medicine on pre- and postoperative nursing care for gastric cancer patients, recommendations were generated for the admission care, preoperative care on the day before the operation, preoperative care on the operation day, immediate postoperative assessment, postoperative care, and discharge care categories. Ideally, each recommendation must be generated based on evidence from randomly controlled experimental research or systematic clinical trials. However, the lack of research evidence regarding the pre- and postoperative nursing care of gastric cancer patients made it very difficult for us to develop recommendations in this way. Thus, more clinical research is needed before future attempts are made to develop evidence-based nursing practice guidelines.
The content validity of the nursing practice guidelines developed herein was tested by nurse experts, who rated 60 out of 64 of the recommendations as valid. Three out of four recommendations with low validity scores were recommendations for the management of antiembolism stockings (AES), which are worn postoperatively to prevent venous thromboembolism. Since very few research outcomes are available in Korea on this topic compared to other postoperative care items such as preventive care of pulmonary complications and pain management, we developed recommendations for preventive care for venous thromboembolism based on the guidelines developed in the developed countries, which are much stricter than those in Korea. Nurse experts made many comments regarding this recommendation because it was very different from current nursing practice in Korea. We therefore modified this recommendation to reflect the current practices regarding preventive care for venous thromboembolism in Korea. AES are currently used to prevent postoperative thromboembolism in Korea; however, there are no guidelines for the management of AES. Thus, the recommendations on AES management developed in this study may be very useful in the future.
When the usefulness and applicability of the guidelines developed herein were evaluated by the nurse experts, average scores were very high, at 4.7 and 4.5 out of 5.0, respectively. For both usefulness and applicability, "helping a patient in a sitting or a semi-Fowler's position and explaining importance of the position" to prevent pulmonary complications in postoperative care was rated at 5.0. This was possible because there is concrete research evidence available for this recommendation. Conversely, pain management was scored lowest for both usefulness and applicability. This could be because clinical nurses lack knowledge on pain assessment and interventions [19,20], do not recognize the importance of pain management, and/or lack the capability to administer pain management [21]. Thus, it is necessary to introduce strategies to improve knowledge on pain assessment and interventions before we introduce the guidelines into the clinical practice. Three out of 4 head nurses and 8 out of 11 staff nurses who evaluated the content validity of the guideline also participated into the evaluation of the usefulness and applicability of the guidelines. Thus, there is possibility of overestimating scores of the usefulness and applicability of the guidelines.
The guidelines developed in the present study cover the total nursing care of gastric cancer patients before and after surgery from the admission to the discharge; it is useful to be able to understand the overall flow of nursing care, and it is helpful to grasp the nursing practices of each domain systematically through guideline algorithms. However, since these guidelines deal with all areas of pre- and postoperative care of gastric cancer patients, some recommendations in the guidelines are not sufficiently specific for nurses to follow. Thus, more specific recommendations for these areas need to be developed in the future.
The guidelines in this study were developed by analyzing 54 research articles. They provide important information and can be used as teaching and training materials-not only for beginner nurses but also nursing students-for the practice of nursing of gastric cancer patients. The guidelines can be implemented in the electronic nursing record system as decision-support system for direct nursing care. If nursing practice guidelines are integrated into the electronic nursing record system, research evidence and patient-specific recommendations can be provided in a pop-up window based on unique patient problems or the nursing diagnosis [22]. In order for this to happen, extensive clinical practice guidelines for different nursing problems should be developed, and the present study represents a milestone toward achieving this goal. If a beginner nurse provides nursing care based on the clinical practice guidelines using a decision-support system, variations in nursing practice can be reduced, which in turn could ultimately reduce variations of patient outcomes.
The guidelines developed in this study were based on research findings and experts' knowledge and validated by nurse experts, which may increase the applicability of the guidelines compared to those developed using only research-based evidence. However, since the nurse experts for our study do not represent every hospital in Korea, this limits the applicability of these guidelines to hospitals other than those where this study was conducted. These guidelines need further validation by different nurse expert groups in different clinical settings if they are to be used more widely.
In order for the nursing practice guidelines to be used for clinical decision-making on direct nursing care, they must be implemented as a part of the electronic nursing record system. In addition, when nursing care is provided based on the recommendations of the practice guidelines, it should be automatically documented in the nursing record. This goal can be achieved by integrating the clinical practice guidelines and algorithms developed in this study into the electronic nursing record system.
Notes
No potential conflict of interest relevant to this article was reported.