|
 |
- Search
| Healthc Inform Res > Volume 16(3); 2010 > Article |
Abstract
Objectives
This purpose of this paper is to introduce the status of the Asan Medical Center (AMC) medical information system with respect to healthcare quality improvement.
Methods
Asan Medical Information System (AMIS) is projected to become a completely electronic and digital information hospital. AMIS has played a role in improving the health care quality based on the following measures: safety, effectiveness, patient-centeredness, timeliness, efficiency, privacy, and security.
Results
AMIS consisted of several distinctive systems: order communication system, electronic medical record, picture archiving communication system, clinical research information system, data warehouse, enterprise resource planning, IT service management system, and disaster recovery system. The most distinctive features of AMIS were the high alert-medication recognition & management system, the integrated and severity stratified alert system, the integrated patient monitoring system, the perioperative diabetic care monitoring and support system, and the clinical indicator management system.
Conclusions
AMIS provides IT services for AMC, 7 affiliated hospitals and over 5,000 partners clinics, and was developed to improve healthcare services. The current challenge of AMIS is standard and interoperability. A global health IT strategy is needed to get through the current challenges and to provide new services as needed.
Asan Medical Center (AMC) was established by the Asan Foundation. The Asan Foundation has placed special importance on medical welfare projects, including establishment of hospitals with professional medical staff and modern medical treatment facilities in areas with limited access to medical treatment. The Foundation recognized the need for a professional hospital that would offer world-class medical treatment and act as a 'hub' for regional hospitals. This recognition the mission led to the opening of AMC on June 23, 1989, with 23 departments and approximately 1,000 beds. Currently, AMC has 2,700 beds and is the largest medical institution in Korea. AMC has approximately 8,000 employees, attends to 10,000 outpatients per day, has an average of 2,600 inpatients daily, and performs about 200 complex surgical procedures every day of the year.
The aspiration and determination of AMC to become a 'patient-oriented hospital' is the driving force behind progress of AMC. AMC has developed integrated healthcare systems and efficient healthcare support systems for a hospital where patients do not have to wait any longer than is necessary and where the privacy of patients is respected. These achievements are made possible through the Asan Medical Information System (AMIS). Medical science and technology have advanced at an unprecedented rate during the past half-century. In tandem has come growing complexity of health care, which today is characterized by more to know, more to do, more to manage, more to watch, and more people involved than ever before. Faced with such rapid changes, health information system has fallen far short in its ability to translate knowledge into practice and to apply new technology safely and appropriately. Health information system is rising as an important tool for improving quality of health care service with unique features [1]. AMIS is also committed to improve quality of health care service, because of our aspiration to be a 'patient-oriented hospital'.
In this paper, we will describe the role played by AMIS in healthcare quality improvement, and propose its distinct features, as defined in the second report of the Institute of Medicine issued in 2001. Healthcare quality encompassed patient safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity [2]. We chose privacy and security instead of equity as one of quality indicators, and we here review the performance of our system with respect to the above-listed criteria, with identification of healthcare quality applications important to these ends.
This section mainly describes the characteristics of main applications and configuration of AMIS, and discusses main issues which should be resolved to improve the quality of health care.
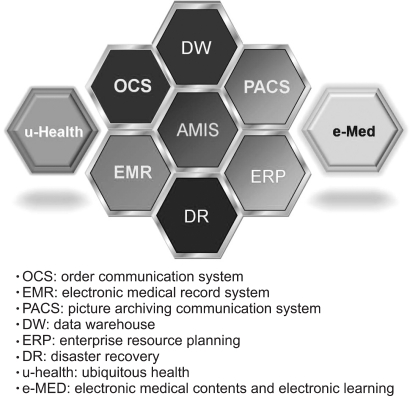
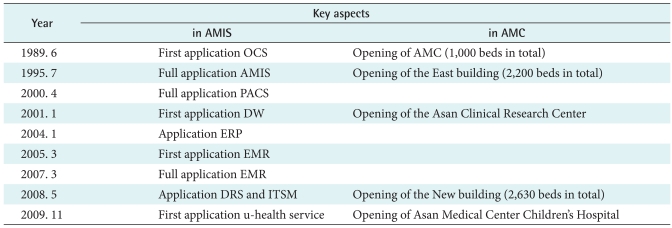
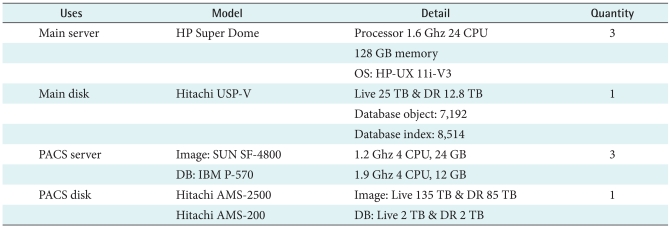
Beginning in 1989, AMC implemented AMIS to become a requisition; slip-less, film-less and paperless hospital, and to efficiently manage hospital. AMIS includes an order communication system (OCS) such like as computerized physician order entry system (CPOE), a picture archiving communication system (PACS), an electronic medical record system (EMR), a data warehouse (DW) and an enterprise resource planning (ERP), and etc. (Table 1, Figure 1). Also a web-based healthcare service (e-AMIS, Web-PACS) is available to partner hospitals and clinics. AMC is affiliated with seven other Korean hospitals and our information-development team offers medical IT services to all colleagues. Most of AMC health IT services is in house built by our medical information-development team.
Both the computational power and the data capacity of our server have been gradually increased over the past 20 years. The main server and disk specifications are shown in Table 2.
AMC OCS has been developed to focus on CDSS based on various references and clinical knowledge. Our clinical decision support areas are well organized; we formally review all antibiotic prescriptions, total parenteral nutrition decisions, chemotherapy calls, identifications of critical pathways, protocol information, and order sets.
Notably, we have used CDSS for more than 10 years to assist in medication decisions. For example, an antimicrobials management system was implemented in 1996 to formalize antibiotics prescription and support. A drug interaction alert system was introduced in 2005 to minimize errors in drug combinations, to provide information on dose limits, to warn of drug interactions, and to provide critical allergy information. Our chemotherapy management system is highly organized and is based on clinical knowledge: this greatly assists our physicians in implementation of optimal anti-cancer chemotherapy regimens and improves the efficiency of cancer patient' care. Recently a pregnancy alert system, termed PLEASE, has also been placed on-line. All of these systems are harmoniously integrated with in our OCS environment.
Our EMR holds all ER, OPD, ward and ICU records. Flow charts allow ward EMR doctors to instantly view patient vital signs using a graphical layout, to evaluate laboratory data, and to consider other clinical findings. A clinical summary information window gives all relevant information at a glance; this includes a list of problems, the operation history, medication information, the OPD schedule, consultant memos, full imaging data, and laboratory information; all are available on an EMR viewer. Each physician has a window allowing recording of notes and disease progression.
Our full PACS package consists of PetaVision (PACS viewer for Clinicians and Radiologists), PetaMotion (an acquisition workstation for non-DICOM modalities including endoscope, and motion frame machines), ROView (a special viewer used by our Department of Radiation Oncology that includes planning information and radiation dose suggestions), PetaPET (a PET/CT image viewer, enabling both PET and CT fusion views), PetaGate (an acquisition workstation), and DICOM implemented servers. Our PACS system supports DICOM 3.0 services which include C-STORE, DICOM worklist and DICOM print.
We developed a DRS to ensure continuity of information service even in a disaster situation, to protect medical records from hardware or data server failure, and to provide a seamless information service during server upgrades. Were a disaster to occur, DRS immediately becomes live. After recovery, all data are transferred to the newly recovered system.
The DRS was developed in 2005, and a software-type DRS running Oracle Data Guard is currently used insulate all AMIS data. The DRS consists of primary database (DB), a logical standby DB, and a physically remote standby DB (the DR DB). The DR DB is synchronized with the primary DB by fast reading of "redo log" data. Each DB is 4 terabytes in capacity. The DR DB is installed on the 8th floor of the Asan Research and Education Building, whereas the primary and standby DBs are located on the 13th floor of the East Building.
To improve IT service quality and user satisfaction, AMC established an ITSM processes and an effectively automated the ITSM system. This has resulted in cost-effective customer support, improved use of IT resources, and increased productivity of IT personnel. All IT processes and related systems comply with our Hospital Evaluation Program and HIPAA Standard Operating Procedures.
AMC was increased almost three times in its size after the opening of the East building in 1994, the New building in 2008, and the number of patients has increased accordingly. To improve the patient care with large patient population, many specialized divisions of centers and clinics were established according to newest modalities and with specialized staffs. For these reasons, complexity and complication in medical service environment caused following issues.
Consolidating IT to healthcare, the new understanding has developed followed by whole new patient care procedures. IT dependency and complexity are increasing continuously in health care [3]. Thus, the provision of stabilized IT service and proactive support are accentuated as first priority. However, in real life it is difficult to operate and evolve IT departments in systematic manner. AMIS has been improved to solve these issues centered on patient safety, business efficiency and process integration.
The Institute for Healthcare Improvement has defined high-alert medications (HAMs) as those that are likely to cause significant harm to a patient, even in intended usage. The Joint Commission International has emphasize that HAM safety muse be improved. However, HAMs are not the only causes of adverse events [4-7]; other problems are also evident. A comprehensive strategy improving medication safety is nonetheless imperative.
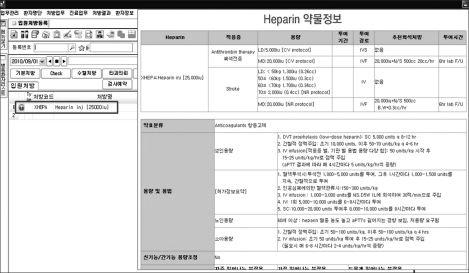
In the interval since February 2008, implementation of the High Alert-Medication Recognition and Management System to Lower Errors and to Secure Safety (HARMLESS) project has effectively reduced the incidence of HAMs-related adverse events at AMC. HARMLESS solution lists were identified by error-type products and contributing factors analysis, and clinical process evaluation using activity diagrams relevant to HAMs. All core messages, adverse drug events, drug interactions, post-medication items to be monitored, similar drugs information, hospital clinical guidelines, and routine drug data, are entered into the OCS. A distinctive red round HAM icon is displayed before the HAM name appears on the OCS screen (Figure 2). The system emphasizes core messages, yet detailed information is also displayed, including information on prior adverse drug events (thus, reports from PI; Performance Improvement experts), hospital clinical guidelines including detailed dose protocols, and routine drug information (provided by pharmacists). Alert-trigger and maximum prescription doses are established using real hospital data.
Our integrated and severity-stratified alert system was developed to manage critical patients information effectively, and to alert medical staff to problems needing attention; we did not wish to disturb the flow of clinical decision-making. Three system input components have been important; Reporting, Censorship and Warning. Data input uses three types of information; Allergy, Infection and Others. The drug allergy input contains drug details, drug ingredients, and allergy symptoms. Infection data include information on antibiotic-resistance, and precautions taken to prevent infection from blood transfusions, air, contacts, absence of isolation, and droplets. Other information may include data on food, and metal allergies. A warning severity is indicated by color; the colors are red, yellow, green, and purple. Red indicates a major problem; yellow, moderate; green, low; and purple, an infection. Integrated alert information appears as a pop-up screen during operation of commonly used computer programs including EMR, OCS, and electronic nursing records (ENR). It is possible to reduce the number of alert messages featuring a combination of allergy data and infection medication. Thus, medical staff can stratify alert severity.
From the patient perspective, what was once a physicianpatient relationship is now more akin to a customer-company interaction. A patient expects his/her hospital to absorb everything relevant to a treatment contract and schedule, and medical history commencing at first contact (possibly by telephone) through to completion of care. A high-quality hospital seeks to deal with these issues and focuses on quality of patient care. An improvement in care quality is synonymous with enhanced patient satisfaction, which is thus paramount. A first-rate hospital information system must prioritize patient service [8]. In particular, long waiting times have a major negative impact on customer satisfaction. AMC has developed an Integrated Patient Monitoring System to deal with this problem. Four monitoring systems are operative; these allow integration of inpatient bed management, an outpatient wait scheduling system, an operation theatre management process system, and an integrated laboratory reservation monitoring system. Not all components are currently operative, but healthcare services will be more efficiently delivered in future (Figure 3).
Our Computerized Perioperative Diabetic Care Monitoring and Support System involves both promulgation of perioperative diabetic blood sugar control guidelines and implementation of a diabetes alert monitoring system. Computerized guidelines for diabetic blood sugar levels are applied to data from diabetics scheduled for operation. A simple text on blood sugar control is offered to all patients and appropriate prescriptions (computer-generated) are listed on a case basis.
Our diabetes alert monitoring system has two input formats. First, physicians may enter data from inpatients with diabetes using real-time clinical information (20 criteria are relevant). Briefly, the parameters may be categorized into three groups, exhibited by patient in whom blood sugar levels are unstable (thus with hyperglycemia or hypoglycemia), by patients for whom prescription of anti-diabetic agents (insulin, oral hypoglycemic agent) have not been effective, or by post-operative patients. The second mode of database entry is available to nurses in charge of monitored inpatients (thus, these healthcare professionals have preferred access). The Diabetes Alert Team reviews monitored inpatient lists and offers recommendations to attending doctors if their prescriptions seem inappropriate.
Our Clinical Indicator Management System gathers raw data from the AMIS environment and summarizes all relevant information compile indicative evidence. Four essential requirements are met. First, system burden is minimized. Second, data access is rapid. Third, changes to the existing system (with which most users are comfortable) are minimized. Finally, a great deal of diverse data must be handled in an (apparently) effortless manner. All useful information is immediately displayed and can be stored in a variety of user-friendly formats. Indicators for AMI, CABG, stroke, and several other conditions are flagged; these are but a few examples of power of the system (Figure 4).
In the interval since December 2008, our PROMISE (Patient Right Observance with Medical Information Security Enhancement Campaign) project has aimed to ensure the security of personal health information contained in AMC. PROMISE involved establishment of an Information Security Management System (ISMS), to ensure international privacy (with security certification) and to establish a privacy/security culture within our institution. An in-house privacy and security task force team developed AMC policy. Our reference text has 10 chapters (including 3 verses), and 67 articles. A Medical Information Security Enhancement Campaign is run annually. In August 2010, AMIS was certified as complying with ISO/IEC 27001:2005. "The ISMS at the ASAN Medical Center's medical information system is certified to comply with Standard ISO 27799".
Any good information system should integrate all units and departments of a hospital. Such communication is critical; absence of discourse encourages errors affecting patient health. Communication improvements are always possible and our ultimate aim is to optimize the quality of patient care, affording maximum responsiveness at minimal cost.
AMIS is a successful provider of IT services for all of AMC, 7 affiliated hospitals and more than 5,000 partner clinics. AMIS has developed near-optimal services addressing patient safety, effectiveness, patient-centeredness, timeliness, efficiency, and privacy and security.
AMIS faces several challenges. Our greatest problem is data standardization; it is imperative to facilitate instant communication among professions with different backgrounds and who (sometimes) do not necessarily agree on optimal treatment regimens. IT standards are constantly evolving and changing [9]. Such IT updates as in Operating Systems change due to security and operability functions can affect our AMIS. These factors are beyond our control. However they may affect any and potentially many parts of our complex and integrated system. We aspire to constantly update and improve our AMIS in spite of changes in both hardware and software technologies to meet our ultimate goal; patient satisfaction. We anticipate there will be more works and dedicated teams to be trained to meet our future growth to meet our objectives.
In addition, storage/retrieval of critical health information that underpins clinical research and treatment is increasingly important. Provision (to patients) of personal health records and u-Health data is now globally popular (and is sometimes mandated by law). Global Health IT strategy is needed to solve these requirements and for the future of AMC. Any global health IT strategy run by a responsible hospital must directly address and welcome such initiatives; AMC is ready to participate.
References
1. Choi IY, Choi R, Lee JH, Choi BG. Implementation of single source based hospital information system for the Catholic Medical Center affiliated hospitals. Healthc Inform Res 2010;16:133-139.



2. Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. 2001. Washington, DC: National Academy Press.

3. Agren M, Winther D. Managing the internal IT function's changing role when outsourcing [Internet] cited at 2010 Sep 2. Available from: http://arc.hhs.se/download.aspx?MediumId=291

4. Federico F. Preventing harm from high-alert medications. Jt Comm J Qual Patient Saf 2007;33:537-542. PMID: 17915527.


5. Kohn LT, Corrigan J, Donaldson MS. To err is human: building a safer health system. 2000. Washington, DC: National Academy Press; p. 86-108.

6. Aspden P, Corrigan JM, Wolcott J, Erickson SM. Patient safety: achieving a new standard for care. 2003. Washington DC: National Academy Press; p. 1-28.

7. Bates DW, Cohen M, Leape LL, Overhage JM, Shabot MM, Sheridan T. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc 2001;8:299-308. PMID: 11418536.



8. Freudenheim M. Many hospitals resist computerized patient care [Internet]. The New York Times 2004;4 06 cited at 2010 Sep 2. Available from: http://www.nytimes.com/2004/04/06/business/many-hospitals-resist-computerized-patient-care.html

9. Demski H, Hildebrand C, Brass A, Jedamzik S, Engelbrecht R. Improvement of cross-sector communication in the integrated health environment. Stud Health Technol Inform 2010;155:95-100. PMID: 20543315.


-
METRICS

-
- 20 Crossref
- 6,033 View
- 37 Download
- Related articles in Healthc Inform Res
-
Blockchain Applications for Healthcare Data Management2019 January;25(1)
Korean Anaphora Recognition System to Develop Healthcare Dialogue-Type Agent2014 October;20(4)
Book Review: Healthcare Analytics for Quality and Performance Improvement2013 December;19(4)
Smart Information System for Gachon University Gil Hospital2012 March;18(1)