I. Introduction
Healthcare has improved greatly over the last decades thanks to medical research, new diagnostic and therapeutic technologies, and evidence-based highly specialized care. However, focus on specialization and single disease has also lead to a fragmentation of patient care. Collaborative care models, often initiated in countries with a strong primary care sector, have therefore been introduced in several parts of the world especially beyond the background of an increase in chronic diseases. To achieve individual health, defined by the World Health Organization as "a state of physical, mental, and social well-being and not merely the absence of disease or infirmity" [1], providing whole-patient care through more integrated approaches is a necessity. This is especially true in the light of an ageing society with shrinking economic resources, when it is increasingly important to provide such integrated support for people suffering from chronic or long-term (often multiple) conditions. As people age, they often suffer from complex and interrelated problems comprising physical, psychological and social health [2]. This requires collaboration between and integration of health and social care to be able to support this group. The nature of the services is very different, and while healthcare is increasingly centralized in health facilities for many reasons, social care is provided in the home or in the nearby locality. In many countries social care management is the responsibility of municipal authorities; in some others it is provided by the same organizations that provide healthcare-but even in these latter the management and record keeping are largely separate, often not least due to legal regulations. This means that at the level of the individual citizen, responsibility for organizing services for a health condition falls to two or more agencies, though the patient seeks a seamless service [3]. Also societal development towards accentuated demands for highly individual, personalized care come into play where not least the Internet has an important role in enabling patients to become better informed. Thus patients and their next-of-kin should be seen as active participants in such a collaborative care process [4]. Informatics is widely regarded as a tool to enable collaborative care involving professional actors from health and social care, informal carers, patients/clients and their relatives. In this context, person-centered collaborative care is seen as a concept addressing both the provision of care over organizational borders between health and social care, and within care teams as well as the changed patient/client-care provider relationship characterized by increased patient/client involvement. With the overall aim to describe the current state of informatics supported collaborative care in this article both, developments in health systems research and in informatics research, are analyzed to point out areas of future research in this highly interdisciplinary field.
1. Collaborative Care: Related Concepts and Definitions
Collaborative care and shared care are often used interchangeably with shared care defined by the European Standard EN13940 as an organizational principle where two or more healthcare providers jointly cooperate to provide healthcare services to a subject of care for a continuing health issue. This organizational principle focuses on joint objectives and responsibilities [5]. Thereby collaborative care involves both agreement between organizations and local co-operation between different care professionals.
Other related concepts are continuity of care, seamless care and integrated care, defined by EN13940 as follows. First, continuity of care is an organizational principle, where one or more healthcare providers deliver several healthcare services to a subject of care. This organizational principle focuses on the time related links between those different services [5]. Second, seamless care indicates a quality principle, focusing on the timely and appropriate transfer of activity and information. This applies when responsibility for the delivery of healthcare services is entirely, or partly, transferred from a healthcare provider to another [5].
Third is integrated care as an organizational principle, encompassing each of continuity of care, shared care, and seamless care at the same time [5]. And last, patient-centered care is a concept that addresses a shift in the relationship between patients and care providers [6], as well as the provision of an integrated view of the entire patient care process, available to all participants. In this sense, shared or collaborative care needs to be integrated in order to be patient- or person-centered [7]. By the author person-centered collaborative care is therefore seen as a concept addressing the provision of care over organizational borders and within care teams as well as the changed patient/client-care provider relationship characterized by increased patient/client involvement.
II. The Health Systems and Organizational Perspective on Collaborative Care
In the United States, collaborative care is regarded as an important aspect to achieve the so called "patient-centered medical home (PCMH)"; i.e., a model for organizing primary care in a way that it is comprehensive, patient-centered, supports co-operation, is responsive to the needs of the individual, and assures quality and safety. The Agency for Healthcare Research and Quality (AHRQ) in the United States has recently published a National Research Agenda for Collaborative Care [8]. AHRQ recognizes the central role of health information technology in successfully operationalizing and implementing the key features of the medical home. Although the above mentioned research agenda is restricted to mental health, it uncovers the lack of a common terminology and the need to develop a lexicon of common terms and components for collaborative care to be able to frame research questions in a consistently understood manner. Further, a framework for collaborative care metrics, where the ability to collect and use practice data represents one of the metrics, is proposed to enable comparative effectiveness research about collaborative care practice [8].
D'Amour et al. [9] reviewed various models and theoretical frameworks of collaboration and found five underlying concepts: sharing, partnership, power, interdependency and process. Interestingly, according to D'Amour et al. [9] there are no models on how to integrate patients into the health care team although patients are the justification for the provision of collaborative care.
Mur-Veeman et al. [10] compared integrated care policies in Europe and stated that a clear proactive policy by national government as well as regional and local authorities matters and that a lack of integrated care policy usually goes hand in hand with a weak primary care sector. Vedel et al. [11] report from the integration of health and social services at the structural level in the province of Quebec, Canada and also point out that despite many reforms and localized initiatives, the Quebec Health System is still struggling with the management of chronic diseases.
For the management of chronic diseases, "Chronic Care Model" of Wagner et al. [12] is pre-dominantly used calling for a system for provision of care involving 7 areas: 1) productive interactions between informed, activated patients, and a prepared practice team; 2) self-management support that empowers patients to take greater responsibility for their own health; 3) delivery system design that requires clarifying roles and tasks to ensure the patient gets the care that is determined to be needed, that all those who take care of a patient have centralized, up-to-date information about the patient's status, and that follow-up is part of standard procedure; 4) decision support tools that assist with ensuring that treatment decisions are made based on guidelines, which are accessible and integrated into the day-to-day practice; 5) clinical information systems that track the care of individual patients as well as populations; 6) organization of health care in systems to create an environment where organized efforts to improve the care of people with chronic illness take hold and flourish; and 7) recognition of the importance of the community in which the system operates, and therefore, creation of alliances and partnerships within the community [13-16].
To summarize, from a health systems perspective a strategic implementation of clinical, technological and organizational changes is required to provide person-centered care. Success factors seem to be a strengthened primary care and shared information systems together with collaboration contracts. The role of patients, family and informal carers requires further analysis.
III. The Informatics Perspective
Collaborative data management between health and social care still depends largely on paper and/or word of mouth and current health informatics standards and terminologies do not yet ensure that the data available to an actor at a given moment can satisfy his/her needs to perform specific care activities [17]. According to Rossi Mori et al. [17] detailed specifications of data sets for e.g., shared care plans or indicators for clinical governance, agreed upon at international level, are still missing. In general, focus has been on standardization of clinical content models [18] and terminologies to achieve interoperability of IT systems but not to support collaborative care processes. On the other hand collaborative tools coming from the fields of telecare and social media are increasingly used to support collaboration between care professionals, between patients and care professionals, within care providing teams and within formal and informal networks. Also emerging technologies for the wellness and prevention sector, including self-management, are used not only to support a single patient but also to communicate with the health care sector [19]. The entire field of consumer health informatics can be placed here [20-22]. However, we are still far from having achieved an effective combination of standardized informatics and collaborative IT tools. Nor have we reached a satisfactory integration of or collaboration between the fields of personal health informatics and clinical informatics. Both fields are relatively well developed and, despite different focus and goals, share common principles and the long-term aim to enhance quality of care for the individual but a number of issues remain to be solved to really achieve holistic health [4].
IV. Examples of Informatics Supported Collaborative Care
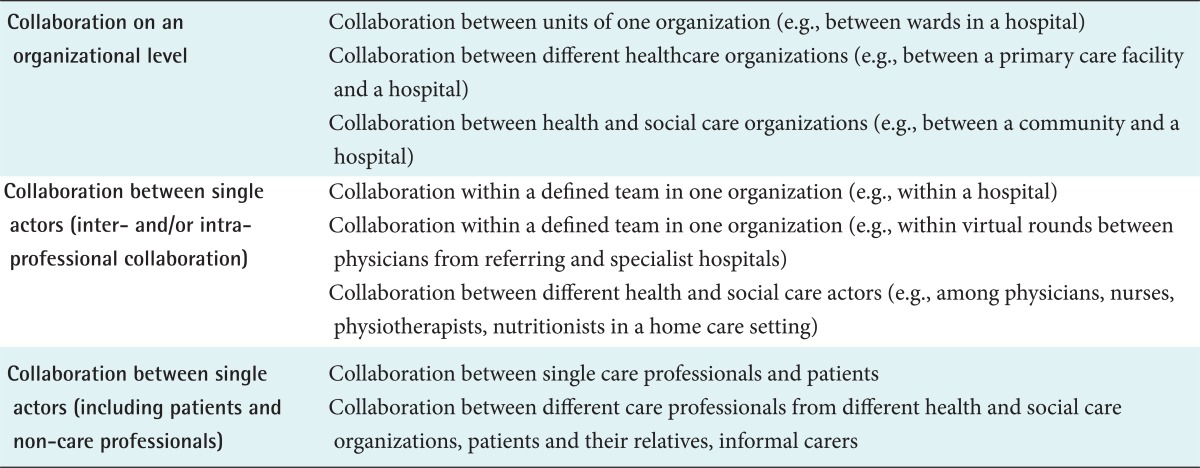
Discussions of concepts and terminology regarding collaborative care in the previous sections show that it is still difficult to grasp the concept and most studies claiming to deal with collaborative care are restricted to healthcare and do not include social care. When it comes to informatics support for collaborative care, we can distinguish between the following situations of collaboration as shown in Table 1.
Collaboration at an organizational level is usually initiated by some sort of contract which also enables structured data management. As an example, when in 2005 the National Board for Health and Welfare issued a regulation mandating collaboration between hospitals and municipalities around a care plan for patients after hospital admittance/discharge [23], local policies were defined and informatics tools for supporting standardized care plans were developed.
From an informatics perspective, many examples focus on the use of standardized messages for communication. Chu [24] reported on standardized data structures for collaborative care messages within care providing teams. They contain scenarios covering referral of patient for nursing and/or medical services, request for aged care placement (long-term or temporary rehabilitation), status reports to the referrer, care completion notification and status query by the referrer to obtain up-to-date client status information while the patient is managed by other members of the collaborative care team.
For collaboration between different actors, Hagglund et al. [25] proposed the definition of interaction points as a starting point for specification of data structures and use scenarios for capturing process knowledge in elderly homecare [26]. They further presented a virtual health record as a mean to share information between primary and social care [27], and a model of a shared care plan based on health informatics standards as a collaborative tool [28]. A similar approach based on predictable attention points (with predictable actors, concerns, activities, and thus highly precise information needs) to be identified within a collaborative organizational context is proposed by Rossi Mori et al. [17].
Ling et al. [29] proposed a route-map to integrated care that includes the development of the necessary infrastructure (including information technology) as one aspect. This route-map starts by analyzing the capability of the existing infrastructure to support integrated care and ends by a new approach to infrastructure supporting continuous improvement.
Such infrastructures exist within a single healthcare maintenance organization (HMO) or a health care system, such as Kaiser [30], Veterans Administration [31]. Maccabi [32] also included information sharing and collaboration through personal health records (PHRs). However, a similar infrastructure coordinating different organizations and health and social care does not exist yet.
V. Barriers and Facilitators for Collaborative Care
Barriers and facilitators for collaborative care resemble those of any large-scale organizational change. Ling et al. [29] reviewed sixteen English Integrated Care Pilots which used a range of approaches to provide better integrated care. The results of this three-year qualitative study found that activities which appear particularly important for delivering integrated care include personal relationships among leaders in different organizations, the scale of planned activities, governance and finance arrangements, support for staff in new roles, and organizational and staff stability. Likely, Hardy et al. [33] found the predominant complexity of the system with a lot of stakeholders having different roles, tasks, interest and power positions as one of the main hinders for integration of services. Also, Canadian experiences showed that although Canada has a long history of health and social services integration at a structural level, the following challenges remain: implementing the reorganization of primary care, successfully integrating primary and secondary care at the clinical level, and developing effective governances and change management [11]. Bates and Bitton [34] uncovered that today's Electronic Health Records (EHRs) lack a number of features required by patient-centered medical homes such as clinical decision support in ambulatory care settings, novel registry tools, real-time specialist consultations, integration of in- and out-patient EHRs, uptake of PHR's, telehealth functionality, ability to deliver quality and efficiency metrics. Although health IT to support collaboration is increasing, the resulting IT systems are not always optimally designed to support clinical collaborative work processes. Wentzer and Bygholm [35] analyzed different IT implementations in Denmark. They studied cases across different health care institutions, across different wards at a university hospital, and across different user-groups in two internal medicine wards. Results showed that the intended effects and visions to provide safer care are not easily realized as unintended consequences such as interaction with the IT system, changed communication patterns, and workarounds may put continuity of care processes at risk and generate interruptions.
To summarize, there is a need for strategic decisions going along with incentives to organizations to perform the required changes for patient-centered care, underpinned by evidence-based informatics tools that guarantee safe and secure data management; and we need incentives for the individual actors to be willing to collaborate and share data, information and knowledge.
VI. Conclusion
This paper summarizes current research regarding informatics support for collaborative care. Being both novel and highly interdisciplinary, the field still lacks a common terminology to mediate between researchers with very different backgrounds and a more detailed research agenda is lacking although different initiatives have been taken in both the United States [8] and Europe [36]. As stated in a recent focus paper published by the European Science Foundation, systematic research activity in the social sciences, at European and national levels, is needed to further the interlinked citizen-focused objectives of: 1) close integration at delivery level of health care and social care support of individual's health; 2) personalization of care delivery including reasonable accommodation of individual choice; 3) ensuring effective use of ICT applications based on user acceptability; 4) bringing processes of consent, delegation, representation, coordination and privacy into the electronic era; 5) ensuring respect for and teamwork with formal carers and the informal care team; 6) ensuring equity in an electronic era regardless of digital literacy, assets and connectivity; 7) examining stable and sustainable models of trusted infrastructure provision; 8) establishing governance, authentication, management, and sustainability principles [36].