Early Experiences with Mobile Electronic Health Records Application in a Tertiary Hospital in Korea
Article information
Abstract
Objectives
Recent advances in mobile technology have opened up possibilities to provide strongly integrated mobile-based services in healthcare and telemedicine. Although the number of mobile Electronic Health Record (EHR) applications is large and growing, there is a paucity of evidence demonstrating the usage patterns of these mobile applications by healthcare providers. This study aimed to illustrate the deployment process for an integrated mobile EHR application and to analyze usage patterns after provision of the mobile EHR service.
Methods
We developed an integrated mobile application that aimed to enhance the mobility of healthcare providers by improving access to patient- and hospital-related information during their daily medical activities. The study included mobile EHR users who accessed patient healthcare records between May 2013 and May 2014. We performed a data analysis using a web server log file analyzer from the integrated EHR system. Cluster analysis was applied to longitudinal user data based on their application usage pattern.
Results
The mobile EHR service named M-UMIS has been in service since May 2013. Every healthcare provider in the hospital could access the mobile EHR service and view the medical charts of their patients. The frequency of using services and network packet transmission on the M-UMIS increased gradually during the study period. The most frequently accessed service in the menu was the patient list.
Conclusions
A better understanding regarding the adoption of mobile EHR applications by healthcare providers in patient-centered care provides useful information to guide the design and implementation of future applications.
I. Introduction
Mobile-based healthcare is undergoing rapid evolution and could prove to be an innovation that would significantly change the future of healthcare. The near ubiquity of mobile technology usage among healthcare providers presents a huge opportunity to improve patient care along the entire value chain. A range of resources has become available, including telemedicine, remote monitoring, and more efficient and comprehensive patient data capture [1]. Recent years have seen an increase in the adoption of mobile devices for healthcare by both healthcare professionals and the general public [2]. The technologies in smartphones and tablets combine mobile communication and computation in a small-sized handheld portable device, facilitating mobile computing at the point of care. Their portability enables use by healthcare providers in a clinical setting. In addition, smart devices also provide health professionals with access to Electronic Health Record (EHR) systems from any location thus facilitating remote consultations and telemedicine [3].
Although the number of mobile EHR applications is large and growing, there is paucity of evidence demonstrating the usage pattern of these mobile applications in healthcare providers. Ours was the first hospital in Korea to deploy a mobile EHR application on a commercial scale (in 2013). We used the information accumulated over the initial 2-year period to analyze adoption rates and usage patterns of healthcare providers who accessed the mobile Ulsan University Hospital Medical Information System (M-UMIS) [4].
This paper explains the deployment process of the mobile application and analyses of the data accumulated during the clinical trial over the previous one year to identify mobile application usage patterns of healthcare providers.
II. Methods
1. Mobile Electronic Health Record Application Development Process
Ours is a 1,050-bed tertiary teaching hospital in Korea, with 1,966 healthcare providers (348 doctors, 907 nurses, and 711 supportive staff). The growing number of patients has increased the demand for sustainable and efficient patient care. The Ulsan University Hospital (UUH) mobile EHR project was initiated in 2012 to provide convenient access to the UUH hospital information system. The application was expected to improve the quality and efficiency of all patient healthcare provisions.
The mobile EHR task force team, consisting of 6 physicians, 2 nurses, and 4 developers, was organized to develop the mobile application in December 2012. Development and beta testing of the mobile application was carried out over 6 months (December 2012 to May 2013) to ensure feasibility and determine the extent of coverage for healthcare providers. The developed mobile application had specific features related to requirements such as patient information (inpatient, outpatient, and emergency), operation schedules, verbal orders, medical consultations, patient searches, duty schedule views, salary views, cafeteria menu, telephone directory, and groupware boards. The personal health record (PHR) system for mobile EHR application has now been in use for over 2 years after beta testing.
2. M-UMIS Structure and Components
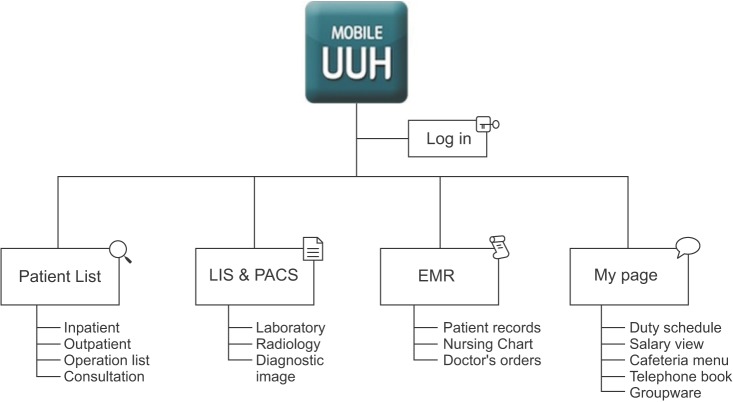
The mobile application, M-UMIS was developed for Android and iOS platforms in native Java programming and Objective-C. User interface (UI) layout objects were designed to support all screen sizes and resolutions of Android and iOS devices. JavaScript Object Notation (JSON) was adapted for the Web-service protocol between mobile devices and the server. All data were transmitted over encrypted Internet connections as HyperText Transfer Protocol over SSL (HTTPS) inside and outside the hospital. Figure 1 shows the communication architecture between the mobile application and hospital electronic system. The main components of the M-UMIS are shown in Figure 2.
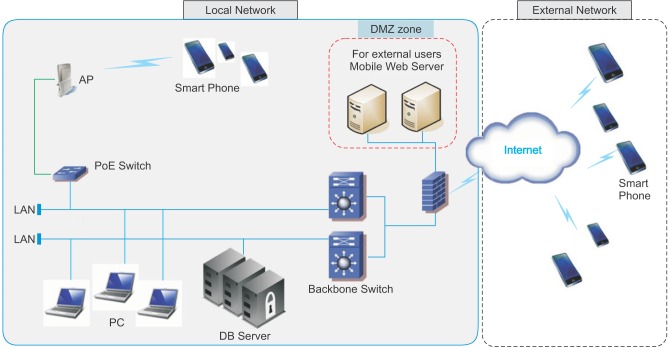
System architecture of mobile Ulsan University Hospital Medical Information System (M-UMIS). DMZ: demilitarized zone, PoE: power over ethernet, AP: access point, DB: database, LAN: local area network.
3. Study Subjects and Statistical Analysis
The extracted access data from the M-UMIS database system was analyzed using Web-based analytical tools (AWStats) from the integrated EHR system [5]. The study included mobile EHR users who accessed patient healthcare records between May 2013 and May 2014. Cluster analysis was applied to longitudinal user data based on their application usage pattern. Our evaluation included a comprehensive analysis of basic demographic data, authenticated visits, most viewed entry, packet data, and logs data. The annual trend was reviewed by analyzing the monthly usage. The study was approved by the Institutional Review Board and Ethics Committee of the hospital.
III. Results
The mobile EHR application enabled healthcare providers to access patient medical information from May 2013 (Figure 3). They could access a variety of patient information, including physicals, lab reports, test results, medical records, and digital diagnostic images, via the mobile application.
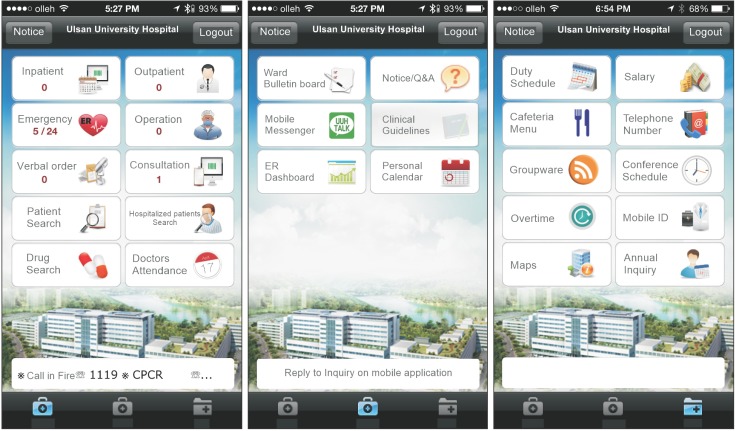
Basic screenshot of mobile Ulsan University Hospital Medical Information System (M-UMIS) application. The application includes patient record and work-related information about patient health record book, test results, drug information, hospital groupware.
1. Demographics of the Study Subjects
A total of 1,394 healthcare providers accessed the M-UMIS between May 2013 and May 2014, including 757 nurses (54.3%), 325 doctors (23.3%), 303 other staff members (21.7%), and 9 pharmacists (0.6%) (Figure 4).
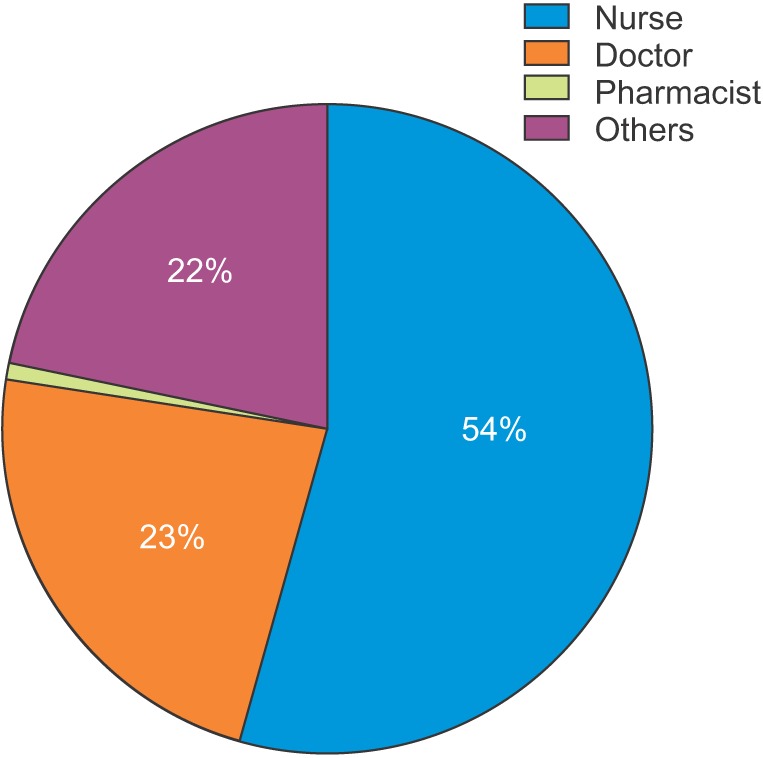
Service user type of accessing mobile Ulsan University Hospital Medical Information System (M-UMIS).
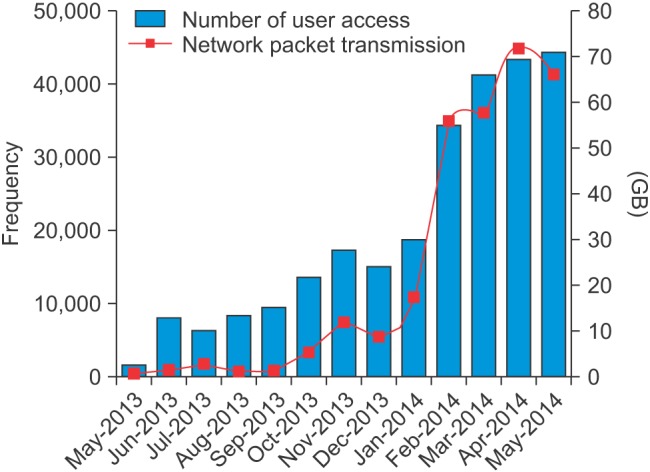
Among the users, the frequency of usage was found to increase gradually during the study period. The most frequently accessed resource was the patient list (Figure 5).

Service menu viewing among users who accessed mobile Ulsan University Hospital Medical Information System (M-UMIS).
Analysis of application usage showed a steady increase in the number of users, accesses, and network packet transmission following the implementation of the service (Figure 6).
2. M-UMIS User Feedback
We received fewer than 70 complaints from healthcare providers who accessed the EHR over the one-year period. The most common complaints were regarding viewing the patient list and test results (Table 1).
IV. Discussion
Various reports have suggested that the use of mobile devices improves patient care by facilitating early and remote expert professional opinion in medical decision-making [6]. However, the diversity of the circumstances that have been targeted has hindered the isolation of specific features that have proven to be efficient. Very few academic studies have analyzed trends and patterns of application usage and access of healthcare providers. This paper aims to evaluate feature-specific usage, which could prove useful in developing a mobile application that satisfies the requirements of healthcare providers.
We have identified the following key intervention strategies to be requisite for an optimal design for deployment of a mobile application: 1) adopting the bring-your-own-device (BYOD) approach, 2) increasing the accessibility of patient information, 3) receiving feedback from users, and 4) maximizing the utilization of desired services.
While introducing the new mobile application, we had to consider several challenging issues, including device fragmentation, inside-out testing, availability of mobile testing tools, and application lifecycle testing [7]. Most healthcare organizations have readily accepted the BYOD approach because of the convenience and potential cost savings associated with allowing employees to bring their own devices to work [89]. The usage rate of mobile devices was about 15 times a day on average for phone calls and a similar rate for emails. Easier communication and increased mobility has been accomplished with the use of smart mobile devices [10]. However, the diversity of devices, operating systems, screen resolutions, memory capacities, and connectivity options is a major hurdle to successful deployment. It is necessary to provide fast connections and stable execution environments that cater to this diversity to ensure optimal functioning. We built the M-UMIS in native Java programming and Objective-C for Google's Android and Apple's iOS operating systems. We also designed the application screens to be compatible with various screen sizes and resolutions. It was made as fast and lightly loaded as possible through native code. However, the hardware compatibility testing for these took 3 months longer than a routine development period.
We also added a push-notification service in the application to improve the accessibility of patient information. Feedback on patients' hospitalization and abnormal laboratory test results are delivered through push-notification by the installed mobile application. This enables a user to check a patient's dynamic condition directly without calling or opening the electronic medical record. Push-notifications deliver more specific and tailored feedback to healthcare providers, which results in better management of the patient's condition.
In an attempt to expand the M-UMIS service across the hospital, we encouraged healthcare providers to use the mobile application. We offered financial support to users to improve service content and performance. Feedback from users was duly considered while solving the problems.
Mobile applications need to reflect user opinions if they are to provide user-friendly services steadily [11]. We have been obtaining a good response from users through feedback and have been improving user participation from the beginning of the open beta test. The users recounted their requirements as follows: free SMS between healthcare providers in the hospital, patient information (inpatient, outpatient, and emergency), operation schedules, verbal orders, medical consultations, patient searches, duty schedule views, salary views, telephone directory, groupware boards, and push-notification services.
The analysis of data from the Web server log file analyzer from the M-UMIS system provided significant results. After nearly 6 months of continuous growth, the number of users accessing the application and network packet transmission has been tremendously increasing since 2014. If a user is involved throughout the system development process, it increases the likelihood of user acceptance of the final version [12]. Therefore, we encouraged our users to participate continually throughout the development process. We also informed our staff regarding the advantages of the mobile application and spread awareness through groupware boards constantly. These efforts increased the access trends to the mobile application.
Successful application implementation requires an increasing number of application users [13]. Each healthcare provider was given instructions on variable use and directions to integrate the mobile application in depth at 8 months post-implementation. As a result, user access and network packet transmission increased sharply. These results are important, as the developer needs to consider the system load during the application deployment process and variables that alter the system load must be factored in.
We also identified the services that were most frequently used in the mobile application. The most frequently viewed service was the patient list, followed by nursing chart, patient medical record, care transition note, lab & imaging test results, and consultations. These findings could be beneficial while planning and prioritizing services during the developmental stage of application deployment.
Telemedicine refers to any healthcare delivery application that uses active media, such as the Internet, mobile platforms, or satellites, for communication between the concerned parties [14]. mHealth or mobile health is defined by the World Health Organization as "medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants (PDAs), and other wireless devices" [15].
The number of smartphone users has been increasing tremendously of late [16]. Mobile devices are becoming an increasingly important platform for healthcare delivery due to 1) the increased adoption of phones with advanced technical capabilities [17], 2) the tendency of people to carry their phones with them everywhere, and 3) the attachment of people to their phones [18]. The latest generation of mobile devices are increasingly viewed as handheld computers rather than as just phones or tablets, due to their powerful on-board computing capability, capacious memories, large screens, and open operating systems that encourage application development [19]. Mobile phones enable healthcare providers to have a comfortable platform that provides many patient-care-related applications and are popular tools for immediate communication with one another. In recent years, researchers from both health sciences and disciplines in computer science, such as telemedicine, ubiquitous computing, and human computer interaction, have developed applications targeting various health categories and conditions. For example, mobile phone applications allow healthcare providers to monitor patients with chronic heart failure and to detect early signs of arrhythmia or ischemia that can indicate an imminent heart attack [2021].
Mobile devices support the delivery of healthcare in a variety of formats. For example, they enable patients and providers to send and receive calls, text messages, access websites, provide clinical decision support, capture and transmit patient data, and house health-focused applications (mobile-specific software) [222324].
Our study has also shown encouraging results for mobile-related information. Some of the mobile-related information included multimedia photo and video. Our application supports the use of camera functions in the EHRs. Smartphones could replace digital cameras as a cost-effective alternative to dedicated hardware equipment in telemedicine. The major components of physical examination of a patient are inspection, palpation, percussion, and auscultation. Unfortunately, telemedicine technologies are limited in time and space and are often unable to cater to a complete physical examination. Physical examination through telemedicine, although limited, can be improved with the upcoming implementation of photo/video transfer by mobile devices [25]. Mobile devices could prove to be better tools for acquiring and sharing patient images compared to the traditional method. The improved quality of digital photographs and video recordings of new mobile devices enables them to work as telemedicine terminals. Our study confirmed the prospects of using photographs through the mobile application to improve healthcare. The rates of packet data transmission and service use pertaining to these functions were found to increase over time since the beta test.
Our study was limited to user access trends primarily during the deployment of the application. It did not include the effects of integrating the mobile application (for example, improved quality of clinical support services, end-user satisfaction). Further evaluation and research are required to better understand the roles and effects of mobile health applications on healthcare. No security-related issues occurred during the study period; however, further research is needed to ensure proper handling of vulnerability and breaches in security, although no security issue arose during the study period.
The findings of our study add to the existing evidence base that would help in the development of integrated mobile services in healthcare.
In conclusion, a better understanding regarding the adoption of mobile EHR applications by healthcare providers in patient-centered care could provide useful information to guide the design and implementation of future applications. This study on integrating mobile health applications is expected to further the development and spread of upcoming mobile application services in telemedicine.
Acknowledgments
We would like to thank BIT Computer Corporation for helping develop the proposed application.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.