Effect of Watch-Type Haptic Metronome on the Quality of Cardiopulmonary Resuscitation: A Simulation Study
Article information
Abstract
Objectives
The aim of this study was to test the applicability of haptic feedback using a smartwatch to the delivery of cardiac compression (CC) by professional healthcare providers.
Methods
A prospective, randomized, controlled, case-crossover, standardized simulation study of 20 medical professionals was conducted. The participants were randomly assigned into haptic-first and non-haptic-first groups. The primary outcome was an adequate rate of 100–120/min of CC. The secondary outcome was a comparison of CC rate and adequate duration between the good and bad performance groups.
Results
The mean interval between CCs and the number of haptic and non-haptic feedback-assisted CCs with an adequate duration were insignificant. In the subgroup analysis, both the good and bad performance groups showed a significant difference in the mean CC interval between the haptic and non-haptic feedback-assisted CC groups—good: haptic feedback-assisted (0.57–0.06) vs. non-haptic feedback-assisted (0.54–0.03), p < 0.001; bad: haptic feedback-assisted (0.57–0.07) vs. non-haptic feedback-assisted (0.58–0.18), p = 0.005—and the adequate chest compression number showed significant differences— good: haptic feedback-assisted (1,597/75.1%) vs. non-haptic feedback-assisted (1,951/92.2%), p < 0.001; bad: haptic feedbackassisted (1,341/63.5%) vs. non-haptic feedback-assisted (523/25.4%), p < 0.001.
Conclusions
A smartwatch cardiopulmonary resuscitation feedback system could not improve rescuers' CC rate. According to our subgroup analysis, participants might be aided by the device to increase the percentage of adequate compressions after one minute.
I. Introduction
The survival rate from cardiac arrest remains poor despite ongoing efforts to improve the ‘chain of survival’ over the past 50 years [1234]. The delivery of high-quality cardiopulmonary resuscitation (CPR), while ensuring chest compression of adequate rate and depth, and allowing full chest recoil, was found to provide a significant survival benefit in previous studies [56]. Although the American Heart Association (AHA) and European Resuscitation Council (ERC) guidelines clearly define how to achieve effective CPR in basic life support (BLS) and advanced cardiac life support (ACLS) [789], maintaining good quality of CC in the field has been reported to be challenging [10].
Therefore, various types of feedback or prompt devices have been introduced to improve the quality of cardiac compression (CC) [11121314]. The most updated AHA and ERC guidelines recommend using audiovisual feedback devices during CPR training to improve skill acquisition and retention [1516]. In the review of interventions to improve CPR quality, not only audiovisual feedback devices but also mobile phones with BLS software or applications also showed favorable outcomes in improving the quality of bystander CPR in the prehospital setting [17]. However, these feedback devices are not as effective as expected in crowded and noisy environments, especially in the hospital setting [18].
Recently, a feedback system using a smartwatch was introduced as a substitute [192021]. Haptic feedback using vibrations from a smartwatch can be more effectively applicable than an audiovisual feedback device in the crowded and noisy environments of emergency settings [22]. In addition, smartwatches can give feedback according to each rescuer and can be worn without disturbing the rescuer's movement.
Although previous studies have demonstrated smartwatches as potential feedback devices for high-quality CC, the outcomes are diverse in terms of CPR quality [192021]. Furthermore, most of these studies have used either visual or audiovisual feedback in laypersons or medical students. Our study aimed to test the effect of haptic feedback using a smartwatch in the delivery of CC by professional healthcare providers. We hypothesized that haptic feedback using a smartwatch would increase the quality of CPR performed by professional healthcare providers.
II. Methods
1. Study Design
We designed a prospective, randomized, controlled, standardized simulation study to determine the effect of a haptic device on CPR quality. The study was approved by the Institutional Review Board of Samsung Medical Center (No. 2018-12-014-001).
2. Study Participants
Twenty participants were recruited from the study site by posting recruitment information on the employee notice board. Medical professionals who were either BLS or ACLS certified were eligible for study participation. Informed consent was obtained from all the participants.
3. Study Protocol
The study was performed with a case-crossover design. On the first visit, the participants were randomly assigned into two groups. The first group performed 2 minutes of continuous CC according to the AHA guidelines with the device (the haptic-first group), and the other group was asked to perform without it (the control-first group). Then, the participants were summoned 1 week later (washout period) to perform CPR as the other group. The study process is illustrated in Figure 1.
4. Description of the Devices
An Ambu Man Basic CPR Manikin was used to collect and store the performance data. The R package ‘peakPick’ was used to detect peaks and intervals of CCs from the performance data. The haptic device used was a Galaxy Gear S3 frontier smartwatch (Samsung Electronics Inc., Seoul, Korea) with a metronome application (Galaxy Store app Wearable Metronome), which is worn at the wrist to provide information with constant metronome-like vibrations at the rate of 110/min (Figure 2). Only the haptic feedback system of the metronome application was used in this study.
5. Measures
We collected information on demographic factors, such as age, sex, job, and CPR experience. As outcome measures, the total number of CCs was counted during 2 minutes. The participants were assigned to two groups according to their CC performance. The 10 best performing participants without the haptic feedback device were defined as the good performance group (GPG), and the next 10 best performing participants were defined as the bad performance group (BPG). Thirty-second intervals in a sequence were demarcated as quartiles 1Q, 2Q, 3Q, and 4Q.
6. Primary Outcome
The primary outcome was the percentage of the number of adequate rate of CC, defined as 100–120/min, with the haptic feedback device. The total number of CCs was counted during 2 minutes, and between 0.5 and 0.6 seconds for one compression was defined as an adequate duration.
7. Secondary Outcome
The secondary outcome was a comparative rate of CC and adequate duration between the good and bad performance groups; data obtained at each 30-second quartile were analyzed.
8. Data Analyses
We described the demographic factors and CPR experience in the two groups. The data were analyzed with the Mann– Whitney U test, χ2 test, Fisher exact test, or generalized estimation equation (GEE) as appropriate. p-values of <0.05 were considered statistically significant. The statistical analysis was executed using SAS version 9.4 (SAS Institute, Cary, NC, USA) and R3.5.1. The odds ratio and 95% confidence intervals (CIs) were estimated from the GEE models that included the main variable and covariates. The primary analysis used to examine the haptic device was the main variant of interest. We examined the following four models: model 1, unadjusted analysis between the haptic and control groups; model 2, adjusted analysis between the haptic and control groups; model 3, adjusted as model 2 with additional adjustment for the quality group; and model 4, adjusted as model 3 with additional adjustment for the 4 quartiles.
III. Results
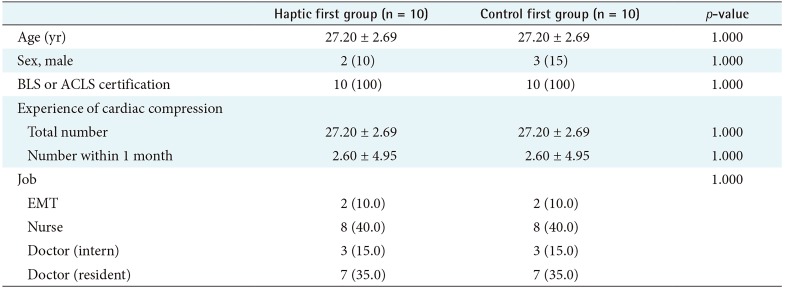
Twenty participants were recruited and then randomized into two groups. Two of the participants were paramedics, 8 were nurses, and 10 were physicians. None of the participants was excluded. The demographic characteristics of the participants are summarized in Table 1. No significant differences were found between the two groups regarding sex, age, and experiences.
1. Primary Outcome
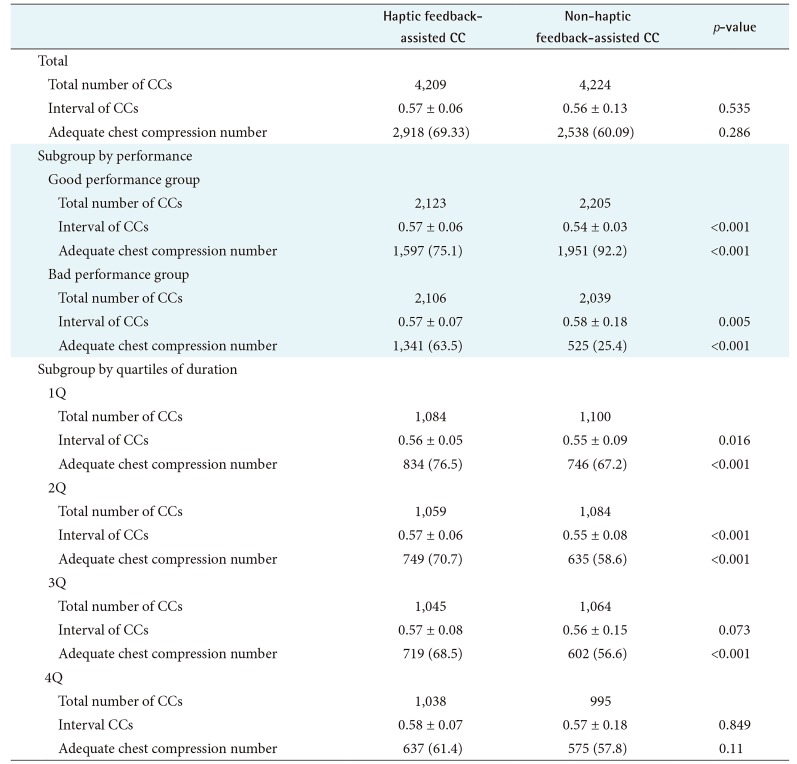
The CC performance results are shown in Table 2. The mean interval of the haptic and non-haptic feedback-assisted CCs did not show a significant difference, and the adequate chest compression number did not show a significant difference. Figure 3 shows a comparison of the timeline graphs of CCs for each participant and the fitted values of the haptic and non-haptic feedback-assisted CCs. The timeline graphs of CCs for each participant were more consistent with the haptic feedback device.
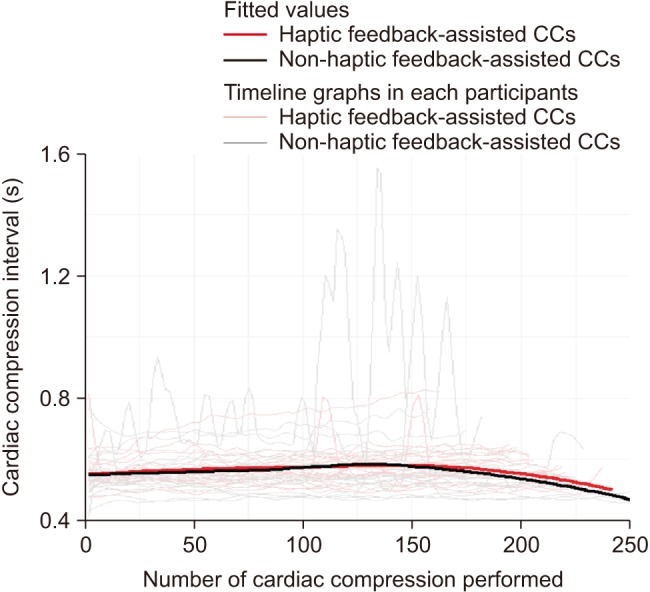
Comparison of the timeline graphs of cardiac compressions (CCs) in each participant and the fitted values of the haptic and non-haptic feedback-assisted CCs.
In the subgroup analysis between the good and bad performance groups, the mean intervals of the haptic and nonhaptic feedback-assisted CCs—good: haptic feedback-assisted (0.57–0.06) vs. non-haptic feedback-assisted (0.54–0.03), p < 0.001; bad: haptic feedback-assisted, (0.57–0.07) vs. non-haptic feedback assisted (0.58–0.18), p = 0.005—and the adequate chest compression number showed significant differences—good: haptic feedback assisted (1,597/75.1%) vs. non-haptic feedback assisted (1,951/92.2%), p < 0.001; bad: haptic feedback assisted (1,341/63.5%) vs. non-haptic feedback assisted (523/25.4%), p < 0.001. Figure 4 shows a comparison of the timeline graphs of CCs for each participant and the fitted values of the good and bad performance groups between the haptic and non-haptic feedback-assisted CCs. The fitted values in the bad performance group were more consistent with the haptic feedback device.
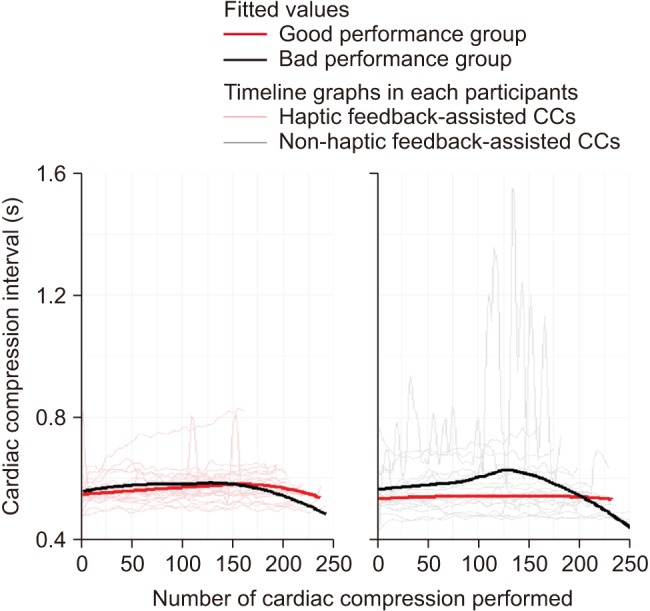
Comparison of the timeline graphs of cardiac compressions (CCs) in each participant and the fitted values of the good and bad performance groups between the haptic and non-haptic feedback-assisted CCs.
In another subgroup analysis, the haptic feedback-assisted CCs showed a generally higher quality from 1Q to 4Q, but no statistically significant difference was found in 4Q, unlike in 1Q and 2Q (Table 2). The mean CC interval and adequate chest compression numbers with and without haptic assistance were the following, respectively: in 1Q, 0.56–0.05 and 0.55–0.09 (p = 0.016), and 834/76% and 746/67.2% (p < 0.001); in 2Q, 0.57–0.06 and 0.55–0.08 (p < 0.001), and 749/70.7% and 635/58.6% (p < 0.001); in 3Q, 0.57–0.08 and 0.56–0.15 (p = 0.073), and 719/68.5% and 602/56.6% (p < 0.001); and in 4Q, 0.58–0.07 and 0.57–0.18 (p = 0.849), and 637/61.4% and 575/57.8% (p = 0.11).
2. Secondary Outcome
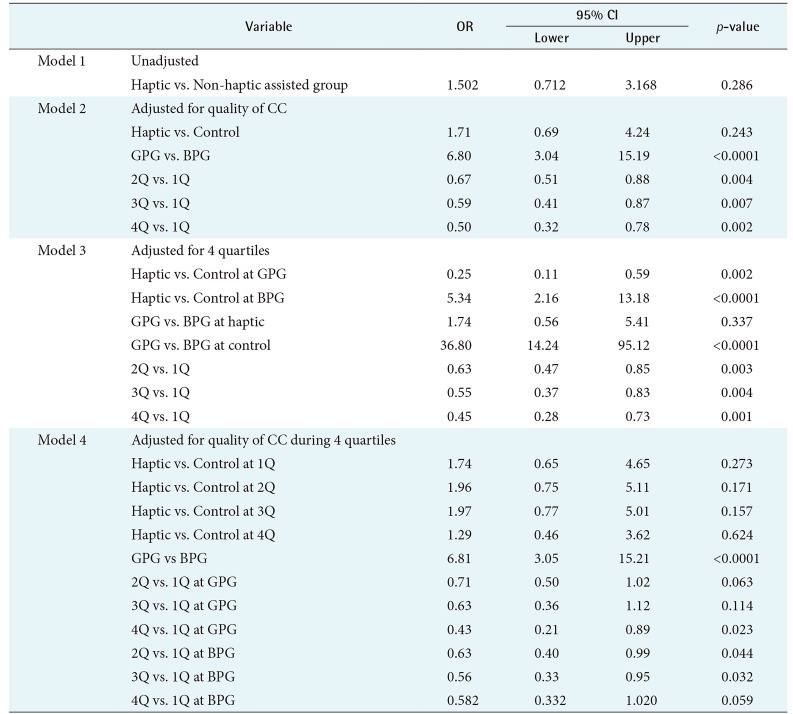
In the GEE analysis, the unadjusted odds ratio for the haptic feedback device assistance shown in model 1 (Table 3) was 1.502 (95% CI, 0.712–3.168). Model 2 shows the adjusted odds ratio (AOR) of the quality group and its positive impact. The AORs were 1.71 (95% CI, 0.69–4.24) and 6.80 (95% CI, 3.04–15.19) for the GPG and BPG, respectively. The AORs for 2Q, 3Q, and 4Q in comparison with 1Q were 0.67 (95% CI, 0.51–0.88), 0.59 (0.41–0.87), and 0.50 (0.32–0.78), respectively. The adjustment for the quality group had a mixed impact on the odds ratio (model 2 vs. model 3) (Table 3). When the haptic feedback device was used, the GPG had a negative impact (AOR = 0.25; 95% CI, 0.11–0.59), but the BPG had >500% increase in the likelihood of CC of adequate duration (AOR = 5.34; 95% CI, 2.16–13.18). In the haptic group, the AOR for the GPG in comparison with the BPG was 1.74 (95% CI, 0.56–5.41). In the control group, the AOR for the GPG in comparison with the BPG was 36.80 (95% CI, 14.24–95.12).
The AORs for 2Q, 3Q, and 4Q in comparison with 1Q were 0.63 (95% CI, 0.47–0.85), 0.55 (0.37–0.83), and 0.45 (0.28–0.73), respectively. Moreover, both the quality and quartile were adjusted in model 4 (Table 3). Each quartile had a positive impact when the haptic feedback device was used (1Q: AOR = 1.74, 95% CI, 0.65–4.65; 2Q: AOR = 1.96, 95% CI, 0.75–5.11; 3Q: AOR = 1.97, 95% CI, 0.77–5.01; 4Q: AOR = 1.29, 95% CI, 0.46–3.62). Both quality groups showed a lower probability of high-quality CC in the time sequence. In the GPG, the AORs for 2Q, 3Q, and 4Q in comparison with 1Q were 0.71 (95% CI, 0.50–1.02), 0.63 (0.6–1.12), and 0.43 (0.21–0.89), respectively. In the BPG, the AORs for 2Q, 3Q, and 4Q in comparison with 1Q were 0.63 (95% CI, 0.40–0.99), 0.56 (0.33–0.95), and 0.582 (0.332–1.020), respectively.
IV. Discussion
This study demonstrated the capability of a smartwatch using a haptic feedback system for CC. No statistically significant difference in the mean CC duration or the proportion of CCs of adequate duration was found between the two groups. However, the haptic feedback device-assisted group showed less standard deviation than the non-haptic feedback device-assisted group. The compression rates without CPR feedback devices were significantly faster than the recommended guidelines [23]. In our study, a large number of participants in the non-haptic feedback device-assisted group tended to perform CCs at a faster or slower rate than that recommended in the guidelines or the haptic feedback device-assisted group. This result implies that CPR quality could be homogeneously controlled by using a smartwatch with real-time feedback, and that it is not affected by rescuer experience or the quality of performance.
Previous studies did not show a significant difference in the CC rate in novice rescuers [2024]. Moreover, even for healthcare professionals, the quality of CPR was suboptimal [25]. In a subgroup analysis, the authors found that the use of the haptic feedback system of a smartwatch significantly increased the proportion of CCs of adequate duration, especially in the poor performance group. To maintain a homogenously good quality of CC during the entire CPR duration, improving the quality CC in the poor performance group might have great clinical importance.
Recently, the use of smartphones as feedback systems to improve the quality of CC has been introduced in several manikin studies [26]. Rescuers need to grasp the smartphone in the palm when performing CC, which may cause errors in the accelerometers depending on their grasping methods [26]. On the other hand, rescuers usually wear smartwatches on the wrist; therefore, if they wear smartwatch, they might overcome the limitations of smartphones. Thus, smartwatches might be better performing feedback devices than smartphones in real-world situations.
The intensity of vibration of smartwatches might vary according to the manufacturer and cannot be customized. The individual perception of vibration might also vary [27]. Excessive intensity of vibration might interfere with CC performance, and a too weak intensity of vibration might not be perceived. Therefore, further investigation in needed to customize and optimize the intensity of vibration via smartwatches for individual users for better CC performance.
This study had several limitations. First, because this was a simulation study on a manikin, the performance of the compressors would be better than that in real-world clinical practice. The authors assumed the feedback from the watch using vibration would be well delivered even in hectic, noisy environments; however, various features in real-world CPR may interfere with compressor performance.
Second, the AHA guideline recommends a 5- to 6-cm depth and full chest recoil in each compression. The participants were familiar with the guidelines but were reminded again of the guidelines before the study. However, the correct hand position, posture, depth, and chest recoil during CCs were not measured in this study.
Third, the participants in this study were recruited from the emergency department of the study site and were all active healthcare professionals with extensive experience in real-world CPR. Therefore, the performance of compressors might be better than that in real-world. Moreover, the baseline characteristic of the participants, such as their height, weight, or athletic performance were not collected, which may have influenced the quality of CPR.
Finally, this study was conducted for healthcare professionals with hands-only CPR with a compression rate range from 100 to 120 per minute. Therefore, the results might not be applicable in the situation of performing compression to ventilation at a 30:2 ratio.
In conclusion, a CPR feedback system using a smartwatch could not improve rescuers CC performance in terms of the ideal range of CC rate in adherence with the CPR guidelines of the ERC or AHA. In subgroup analysis, the initial compression period of one minute after starting CC might be helpful using a smartwatch to increase the percentage of adequate compression.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.