Digital Health Technology-Based Patient-Centered Seamless Care Model for Chronic Disease Management after Cancer Treatment
Article information
Over the past several decades in South Korea, the number of cancer survivors has increased to more than 1.1 million [1]. This has been accompanied by an increase in non-cancer mortality from chronic diseases in cancer patients [2], and therefore, the importance of chronic disease management after cancer treatment has garnered attention.
Survivorship care models for cancer patients’ healthcare have been proposed in countries throughout the world [3–5]. In South Korea, projects linking local clinics and community-based healthcare resources are being conducted at the national level. For example, the health information exchange (HIE) pilot project is establishing an electronic transmission/reception system for patient medical records [6,7], the primary care chronic disease management (PCDM) pilot project is laying the foundations for a comprehensive chronic disease management system based on local clinics [6], and the personal health records (PHR) project is building a health management platform by standardizing, integrating, and relating personal medical information [8].
Although a system for managing chronic diseases through linkage between local primary care clinics and cancer treatment hospitals has been developed, limited information is currently being exchanged through this system. Cancer survivors tend to return to the hospitals where they received cancer treatment for chronic disease management [9]. However, effective cancer patient health management necessitates the establishment of a patient-centered, community-based health management system that is connected with the previously developed health management system.
Service Model for the Management of Chronic Diseases in Cancer Patients
As shown in Figure 1, we propose a policy model for seamless patient-centered chronic disease management after cancer treatment in Korea that involves linkage among the cancer treatment hospital, local primary care clinic, and home-based self-management. The new HIE system, which integrates the HIE pilot project and the PCDM pilot project at primary care clinics, is expected to play a role in efficient periodic monitoring of disease management and health management education for patients. Cancer treatment hospitals play a role in patient management, but mainly focus on cancer treatment. Automatically linking patient treatment information in a standardized format between cancer treatment hospitals and primary care clinics through the new HIE system would enhance clinicians’ understanding of cancer patients’ health conditions and facilitate patient-customized healthcare. Seamless patient monitoring services could also be enabled by transmitting/receiving PHR data or patient lifelog data, measured by Internet of Medical Things (IoMT) devices, and linking the data to a cloud-based chronic disease management platform [10].
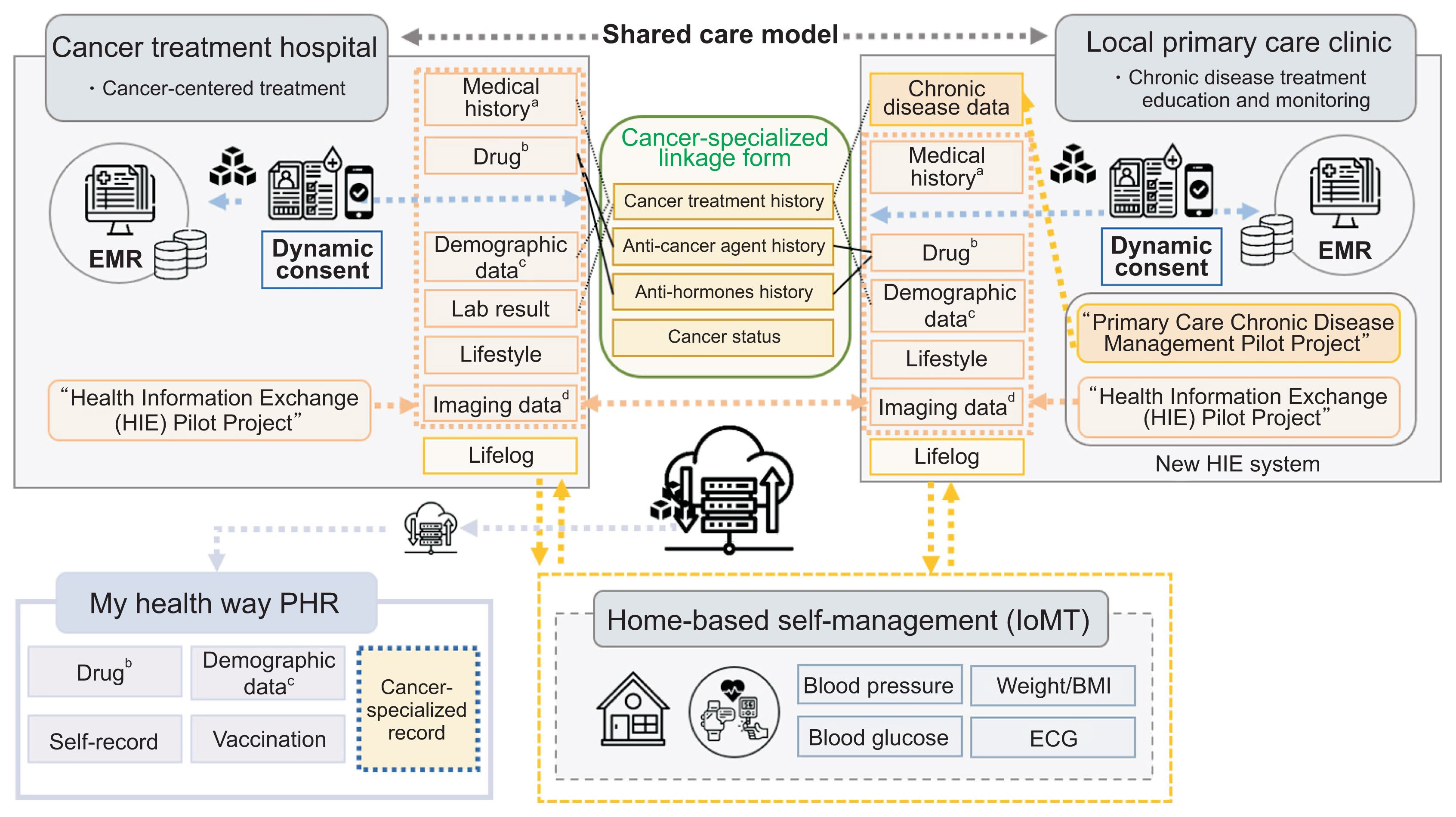
Proposed health information linkage service model for chronic disease management after cancer treatment. EMR: Electrical Medical Record, IoMT: Internet of Medical Things, BMI: body mass index, ECG: electrocardiogram. aPatient history and treatment history, bmedication history, cbasic information of the patient, dmedical imaging information: radiology information, digital pathology data, DICOM data, etc.
In order to apply this model to the actual medical delivery system, consent for the provision and utilization of patients’ personal information is required in accordance with Article 16, Paragraph 1 of the Domestic Bioethics Act [11]. Therefore, dynamic consent (DC) is applied in the new HIE pilot project platform, where the consent of the patient is obtained via an opt-in device requiring users’ clear consent for the collection and use of their data [12]. It is also necessary to establish a health management system for cancer patients in an environment where information security is guaranteed by utilizing blockchain technology for DC.
As shown in Figure 1, the Cancer-Specialized Linkage Form is a form developed in this study that will be introduced into the new HIE system. Additional items for chronic disease management after cancer treatment were selected by analyzing the discharge plan form through a pilot study by the National Cancer Center [13]. Cancer diagnosis history, cancer treatment history, medication history, and basic cancer diagnosis and treatment information need to be added for linkage. In the medication history category, additional information needs to be collected on patients’ history of taking anti-cancer and anti-hormonal agents. In more detailed subcategories, information on the round of administration, type, cycle, and total administration period should be collected for anti-cancer agents, and the type and administration start date should be collected for anti-hormonal agents. This information can be automatically linked from cancer treatment hospitals to primary care clinics, meaning that there will be no additional workload for primary care centers.
In order to establish a seamless health management system for cancer patients, we propose a direction for improving the existing medical information exchange system. The PCDM pilot project, which focuses on managing items related to chronic diseases, and the HIE pilot project, which deals with comprehensive health data, need to be integrated to reduce the workload of primary care clinics. Adding the cancer-specific healthcare items presented in this paper to the integrated platform will enable systematic chronic disease management after cancer patients return to the community. Simultaneous linkage of self-management items at home through the integration of patients’ IoMT devices via the introduction of a pilot project for fee application would enable customized full-cycle health management centered on cancer patients’ personal health information. In the future, it is also expected that institutional linkage will be possible for the patient-centered My HealthWay PHR project, which is being promoted by the government.
Acknowledgments
This study was funded by a grant from National Cancer Center Grant NCC-2210870 (No. NCC-2210870) and the Korea Health Promotion R&D Project, funded by the Ministry of Health & Welfare, Republic of Korea (No. HS20C0093).
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
References
Bioethics and Safety Act, Article 16-1 Law (32268) (December 28, 2021)
