Factors Influencing the Acceptance of Distributed Research Networks in Korea: Data Accessibility and Data Security Risk
Article information
Abstract
Objectives
Distributed research networks (DRNs) facilitate multicenter research by enabling the use of multicenter data; therefore, they are increasingly utilized in healthcare fields. Despite the numerous advantages of DRNs, it is crucial to understand researchers’ acceptance of these networks to ensure their effective application in multicenter research. In this study, we sought to identify the factors influencing the adoption of DRNs among researchers in Korea.
Methods
We used snowball sampling to collect data from 149 researchers between July 7 and August 28, 2020. Five factors were used to formulate the hypotheses and research model: data accessibility, usefulness, ease of use, data security risk, and intention to use DRNs. We applied a structural equation model to identify relationships within the research model.
Results
Data accessibility and data security were critical to the acceptance and use of DRNs. The usefulness of DRNs partially mediated the relationship between data accessibility and the intention to use DRNs. Interestingly, ease of use did not influence the intention to use DRNs, but it was affected by data accessibility. Furthermore, ease of use impacted the perceived usefulness of DRNs.
Conclusions
This study highlighted major factors that can promote the broader adoption and utilization of DRNs. Consequently, these findings can contribute to the expansion of active multicenter research using DRNs in the field of healthcare research.
I. Introduction
Efforts to conduct diverse research through multicenter collaborations have increased the capacity for exchanging healthcare-related data, as exemplified by distributed research networks (DRNs) [1]. DRNs are a method that transmits analysis code to each institution, using only the results, without directly providing the original data [2]. Therefore, DRNs have the advantage of yielding research results as though all the data have been gathered and analyzed, but without creating security risks since the original data remain within the organization [3].
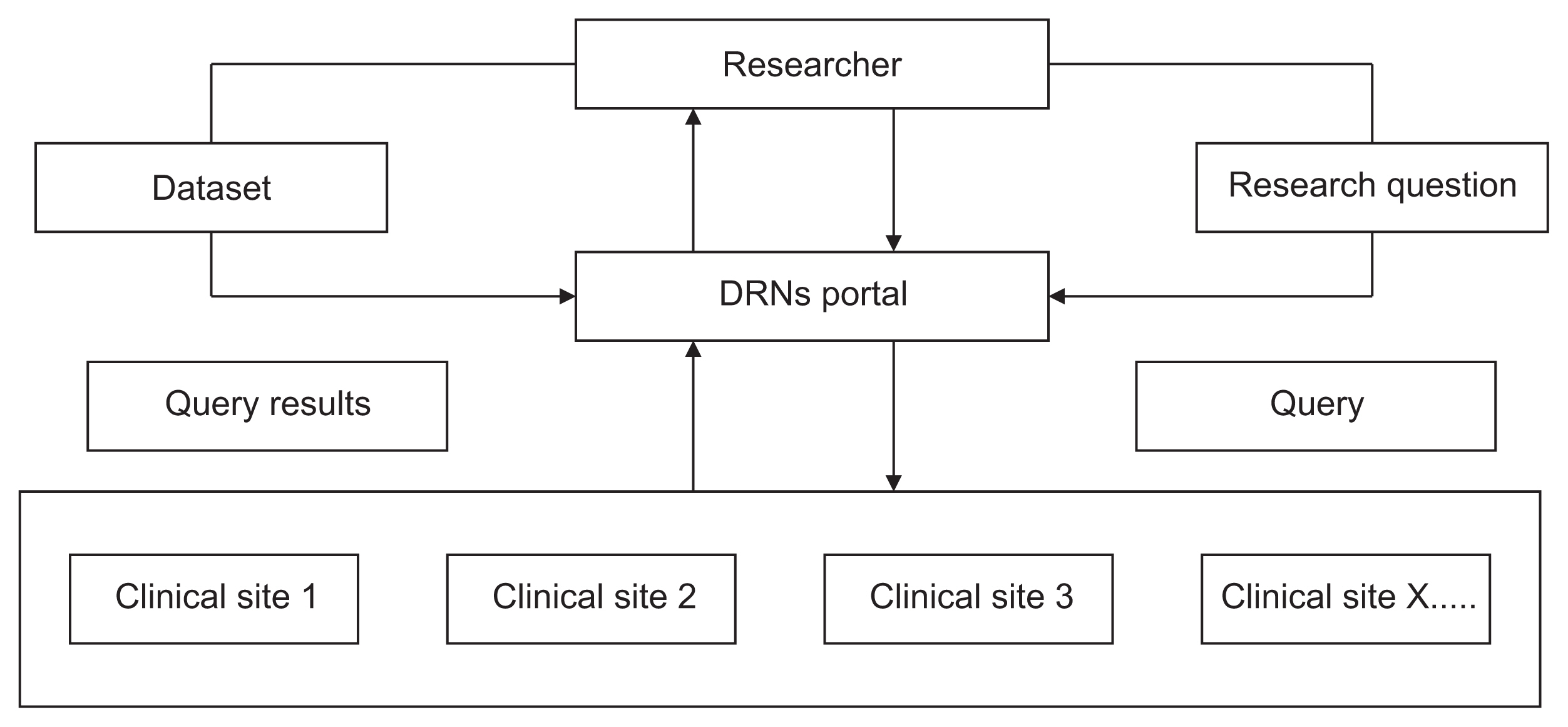
For example, DRNs transform medical data, such as Electronic Medical Records (EMR), into a standardized data model using common terms. Subsequently, DRNs offer a data catalog to researchers from other institutions, which can be accessed and utilized in their studies. The DRN administrator then reviews and approves the proposed research, implements the analysis code supplied by the researcher, and sends the results back to the researcher, as depicted in Figure 1 [4].
Security concerns prevent the sharing of EMR data for multicenter research. However, each institution owns the data within DRNs, which can be utilized for research purposes. The primary advantage of DRNs is their ability to facilitate multicenter research by providing access to multicenter data that is typically difficult to obtain [4]. For this reason, DRNs have been used in various healthcare fields [2,5,6].
Korea utilizes government-led DRNs, namely (1) the Health and Medical Big Data Platform of the Ministry of Health and Welfare [7] and (2) Medical Record Observation and Assessment for Drug Safety (MOA Net) of the Korea Institute of Drug Safety & Risk Management [8]. The use of these DRNs supports the need for the acceptance of multi-center research.
Although DRNs have advantages, it is crucial to understand researchers’ acceptance of DRNs to ensure their effective application in multicenter research. Consequently, we sought to identify the key factors influencing the introduction of DRNs in Korea. By examining previous research related to the technology acceptance model (TAM) in healthcare, we aimed to gain deeper insights into the acceptance of DRNs.
1. Hypotheses and Research Model
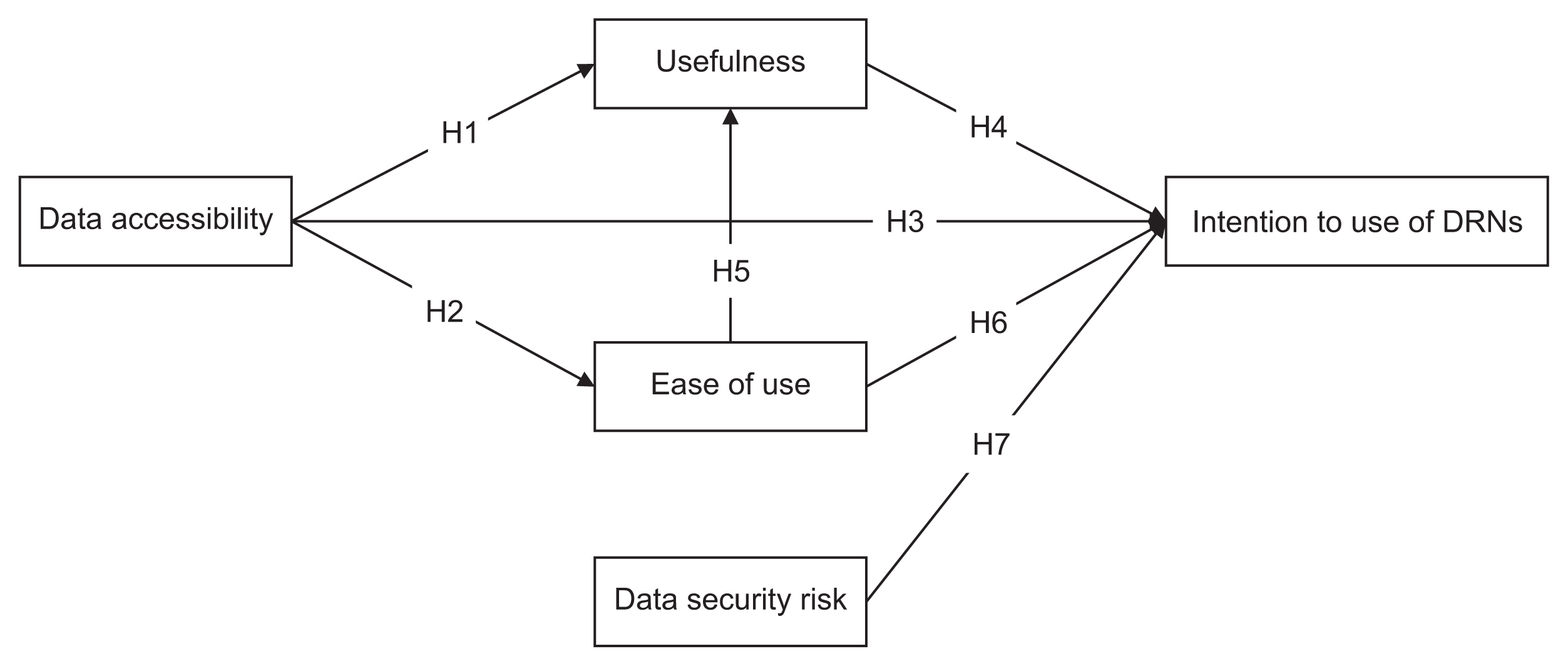
We formulated our hypotheses and research model based on five key factors: data accessibility, usefulness, ease of use (EOU), data security risk, and the intention to use DRNs. These five factors, which influence the acceptance of DRNs in healthcare, were derived from the TAM [9] and previous related studies [10–14].
1) Data accessibility
In this study, data accessibility refers to the perceived extent to which the use of DRNs can provide accurate and appropriate data from other institutions [10,15]. Data accessibility, particularly in relation to medical records, has been reported to enhance clinical outcomes in telemedicine [10,15]. Similarly, the utilization of diverse data from multiple institutions is crucial for research in the healthcare industry. However, hospital data possess certain characteristics that prevent data from being shared externally. Consequently, these institutions must have access to trustworthy multicenter data. We therefore suggest that increased data accessibility will inevitably result in greater usefulness and ease of use. Furthermore, higher data accessibility is likely to lead to a stronger intention to use DRNs. In accordance with these observations, we propose the following hypotheses:
H1: Data accessibility has a positive relationship with the usefulness of DRNs.
H2: Data accessibility has a positive relationship with the ease of use of DRNs.
H3: Data accessibility has a positive relationship with the intention to use DRNs.
2) Usefulness, ease of use, and intention to use DRNs
Usefulness refers to the degree to which a researcher believes that utilizing DRNs would improve the quality and efficiency of their research [11,15]. EOU denotes the level of ease that a researcher associates with the use of DRNs [11,12]. Intention to use means the degree of a researcher’s behavioral intention to use DRNs [13,14]. Both usefulness and EOU are recognized as significant factors in the acceptance of technology [14]. As a result, these two factors have been applied in various healthcare contexts [11,12]. Moreover, previous literature has emphasized that usefulness and EOU lead to the intention to use DRNs [13,16]. It has also been suggested that EOU can enhance perceived usefulness [15]. Given these established relationships, it is anticipated that researchers will employ DRNs if they perceive them as beneficial to healthcare research and easy to use. Therefore, we propose the following hypothesis:
H4: Usefulness has a positive relationship with the intention to use DRNs.
H5: Ease of use has a positive relationship with the usefulness of DRNs.
H6: Ease of use has a positive relationship with the intention to use DRNs.
3) Data security risk and the intention to use DRNs
In this study, data security risk refers to the extent of a researcher’s concern that the utilization of DRNs could lead to increased data exposure and unauthorized data use [1,4]. Data use in a technological context carries the risk of data exposure [12,17,18]. Specifically, since EMR data involve protected health information, there has always been a dialogue surrounding data exposure and the concerns it raises [1]. Privacy and security policies also pose significant concerns for researchers and providers in terms of accepting DRNs [19]. In other words, given that DRNs handle data, data security risk is viewed as one of the key issues associated with DRNs [1,4]. Therefore, the following hypothesis is proposed:
H7: Data security risk has a negative relationship with the intention to use DRNs.
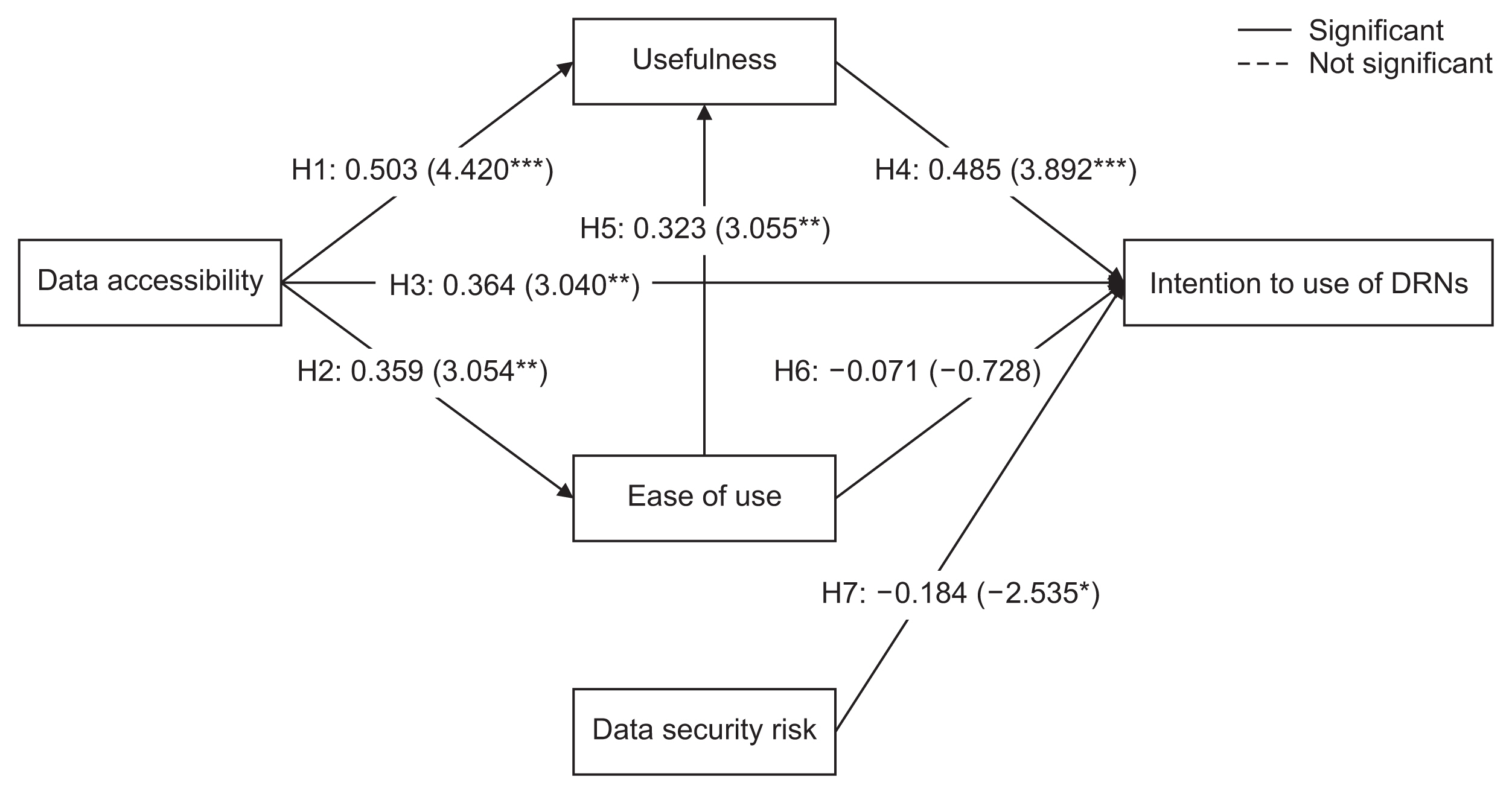
Based on the above literature and hypotheses, a research model was developed and is presented in Figure 2.
II. Methods
1. Participants
We conducted a survey among individuals in hospitals and universities, including professional researchers, doctors, nurses, pharmacists, and students in both master’s and doctoral healthcare programs, utilizing snowball sampling [20]. This method begins with a small, intentionally or expediently selected sample, which gradually expands to form a larger sample [21]. Snowball sampling is useful when it is difficult to find study subjects belonging to the population being examined. Thus, the online survey link was initially distributed to 10 researchers in the healthcare field who were able to participate. Online surveys were conducted from July 7 to August 28, 2020. Of the 151 completed surveys, two were excluded because they were incomplete. Thus, the final sample included data from 149 respondents.
2. Measures
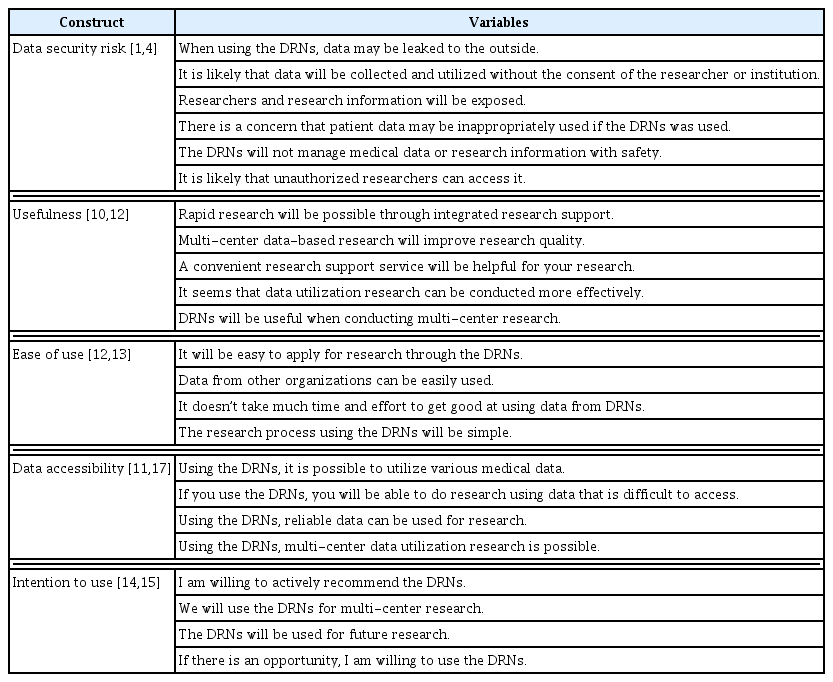
Table 1 presents the specific items included in the questionnaire. The total questionnaire comprised 23 items: six items on data security risk, five items on usefulness, four items on intention to use DRNs, four items on ease of use, and four items on data accessibility. All questions utilized a 5-point Likert scale.
Each item was first derived from the prior literature [1–4,9–15] and subsequently adapted to suit the subject of DRNs. The questionnaire was further supplemented by a team of four researchers, comprising two experts in medical informatics, one researcher with a master’s degree, and one researcher at the undergraduate level.
3. Statistical Analyses
We identified the factor structure of our research model. Subsequently, we assessed the reliability of all constructs using Cronbach’s alpha. We then carried out a principal component analysis with varimax rotation and performed a confirmatory factor analysis (CFA) to evaluate the validity of each construct. We examined the construct average variance extracted (AVE) and reliability (critical ratio [CR]) scores to establish convergent validity, and also assessed discriminant validity. Finally, we tested the hypotheses of our research model. We utilized R to analyze the descriptive statistics and internal consistency. Additionally, we employed a structural equation model (SEM) to identify the relationships between model parameters, again using R. The R package lavaan (version 0.6–5) was used for the SEMs [22].
4. Ethics
We secured research approval from the Institutional Review Board of the Catholic University (No. MC20QISI0066). All data from respondents was anonymized. Approval for participation was obtained online.
III. Results
1. Participants’ Characteristics
The demographic characteristics of the 149 respondents are presented in Table 2. The sample was nearly evenly split between males and females. The plurality of respondents (38.26%) were in their 30s. In terms of occupation, 37.58% of respondents were researchers, while 23.49% were professors. Furthermore, 39.60% had less than 5 years of experience in their respective fields, and 25.50% had less than 10 years. The respondents were primarily affiliated with universities (44.97%) and hospitals (42.95%). Geographically, 81.88% of respondents were based in the capital region, which includes Gyeonggi Province and Incheon City. In relation to research fields, 42.28% were involved in medicine and pharmacy, while 22.15% were engaged in the field of convergence. Notably, only 11.41% of respondents had experience with DRNs.
2. Reliability and Validity
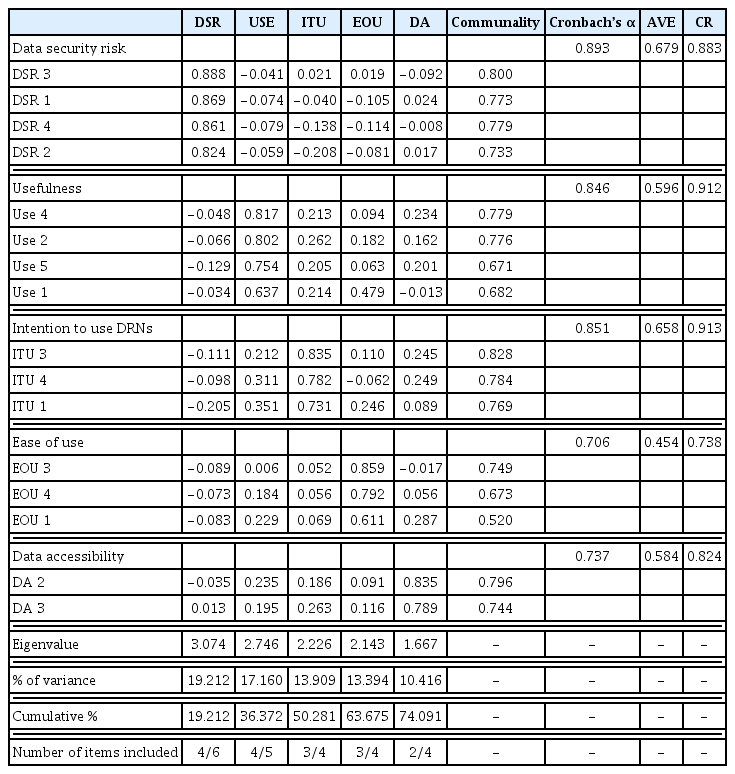
We conducted a principal component analysis with varimax rotation (Table 3). All variables demonstrated no crossloadings exceeding 0.6. We verified the presence of all variables with eigenvalues above 1.0, which represented 74.091% of the total variance in the model. The communality varied between 0.706 and 0.893, and all variables met the 0.50 threshold. As a result, we confirmed that all constructs were distinct unidimensional scales.
Next, we assessed the reliability of all constructs using Cronbach’s alpha. The internal consistency values for all constructs were significant, and all variables were deemed reliable: α = 0.893 for data security risk, α = 0.846 for usefulness, α = 0.851 for behavioral intention to use DRNs, α = 0.706 for EOU, and α = 0.737 for data accessibility. The internal consistency values for the two constructs exceeding 0.70 suggest that these items demonstrated good internal consistency reliability [23].
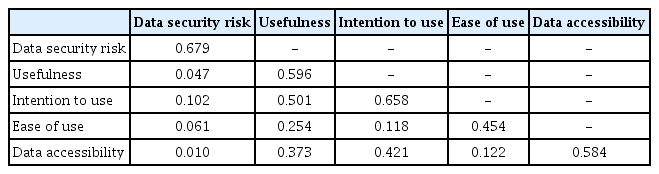
The CFA results indicated that all values met the recommended threshold: chi-square/degree of freedom (χ2/df = 1.351), comparative fit index (CFI = 0.970), root-mean-square error of approximation (RMSEA = 0.049), and Tucker-Lewis index (TLI = 0.962). Convergent validity was evaluated for each construct. All variables had an AVE loading above 0.50 (0.679 for data security risk, 0.596 for usefulness, 0.658 for behavioral intention to use DRNs, 0.454 for EOU, and 0.584 for data accessibility) [24]. All variables had a CR score above 0.70 (0.883 for data security risk, 0.912 for usefulness, 0.913 for behavioral intention to use DRNs, 0.738 for EOU, and 0.824 for data accessibility) [25]. Finally, variables that demonstrated validity and reliability in the CFA results were selected for analysis: four out of six items for data security risk, four out of five items for usefulness, three out of four items for behavioral intention to use DRNs, three out of four items for EOU, and two out of four items for data accessibility.
Table 4 displays the results for discriminant validity. To ensure discriminant validity, the square root of the AVE must exceed the correlation with each construct [15]. The square root of the AVE surpassed the corresponding inter-construct correlations, thereby confirming discriminant validity.
3. Hypothesis Testing
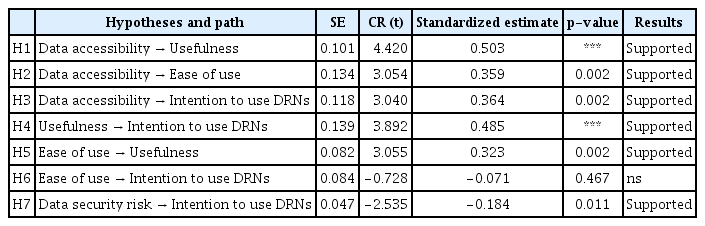
We evaluated the fit of the structural model using various goodness-of-fit measures. The results fell within acceptable parameters: χ2/df = 1.387, CFI = 0.967, RMSEA = 0.051, and TLI = 0.958 (Table 5).
Figure 3 presents the structural path diagram, while Table 6 shows the SEM results for the hypotheses. All hypotheses received support, with the exception of H6. There was a positive relationship between data accessibility and usefulness (β = 0.503, p < 0.001), EOU (β = 0.359, p < 0.01), and the intention to use DRNs (β = 0.364, p < 0.01). Usefulness had a positive impact on the intention to use DRNs (β = 0.485, p < 0.001), and EOU positively influenced usefulness (β = 0.323, p < 0.01). Lastly, data security risk was negatively associated with the intention to use DRNs (β = −0.184, p < 0.05).
IV. Discussion
This study aimed to identify the factors that influence the acceptance of DRNs in Korea. To achieve this, we constructed and validated a research model that incorporated five key influencing factors. These factors included data accessibility, usefulness, EOU, data security risk, and the intention to use DRNs. All of our hypotheses were supported, with the exception of H6, which proposed that EOU impacts the behavioral intention to use DRNs.
First, we found that data accessibility was paramount to the use and acceptance of DRNs. That is, the more accessible the data was perceived to be, the more researchers acknowledged the utility of DRNs for their research and the easier they found its use. These findings imply that data accessibility significantly influences the intention to use DRNs. Moreover, DRNs prove to be effective in studies that necessitate extremely large sample sizes or in studies involving rare exposures [3,4]. Researchers intending to use DRNs often aim to access data that is typically hard to obtain or involves a large volume of data. Consequently, it is essential to enhance DRNs to allow researchers to easily comprehend the data they wish to use and to select and utilize it effectively. In the context of DRNs, it appears necessary to simplify data selection when dealing with complex data from other institutions. This is due to the potentially intricate composition and structure of data from each medical institution. Therefore, offering a visualization of the data that researchers can select within the DRN could potentially increase effective data utilization.
Second, we identified the importance of data security in the acceptance of DRNs. While numerous prior studies have addressed policies and procedures for the secure transfer and storage of study results [2,3,26], there appears to be ongoing concern among researchers about the security risks linked to data usage. Consequently, to encourage the active utilization of DRNs, it is necessary to develop a range of security technologies that can alleviate these data security risks.
Third, usefulness was found to play a role as a partial mediator in the relationship between data accessibility and the intention to use DRNs. This reaffirms the importance of usefulness in the acceptance of DRNs, aligning with prior research that indicates a positive correlation between perceived usefulness and the intention to use technology [27–29]. However, EOU did not serve as a mediator between data accessibility and the intention to use. This may suggest that the majority of respondents are experts in their respective fields, and thus, the ease of use was not a significant factor in their acceptance of DRNs. Nevertheless, it is worth noting that as data accessibility improved, so did the ease of use. Therefore, EOU should not be disregarded in the development of DRNs, as it impacts usefulness, which is consistent with the findings of previous studies [15,30].
Despite these significant findings, there are some limitations that should be taken into account. Firstly, while various DRNs are available in Korea, they are not yet widely used as a standard research method. As a result, the number of respondents who had experience with DRNs was limited. Future studies should aim to include more experienced DRN users. Secondly, despite the use of SEM, the volume of data collected was relatively small. This may have been due to the participation of medical field researchers, who might have found it challenging to complete the questionnaire. Even though the sample size was small, the model fit was excellent. Nonetheless, further research with a larger number of respondents is needed to validate these findings.
Despite these limitations, our study highlighted major influencing factors that could contribute to the expansion and utilization of DRNs. Therefore, these findings will aid in promoting active multicenter healthcare research employing DRNs.
Acknowledgments
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (No. HI19C0870). This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. NRF-2022R1G1A1011635).
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.