Using Online Respondent Driven Sampling for Vietnamese Youths' Alcohol Use and Associated Risk Factors
Article information
Abstract
Objectives
The average alcohol consumption per capita among Vietnamese adults has consistently increased. Although alcohol-related disorders have been extensively studied, there is a paucity of research shedding light on this issue among Internet users. The study aimed to examine the severity of alcohol-related disorders and other associated factors that might predispose individuals towards alcohol usage in a sample of youths recruited online.
Methods
An online cross-sectional study was conducted with 1,080 Vietnamese youths. A standardized questionnaire was used. Respondent-driven sampling was applied to recruit participants. Multivariate logistic and Tobit regressions were utilized to identify the associated factors.
Results
About 59.5% of the males and 12.7% of the total youths declared that they were actively using alcohol. From the total sample, a cumulative total of 32.3% of the participants were drinking alcohol, with 21.8% and 25.0% of the participants being classified as drinking hazardously and binge drinkers, respectively. The majority of the participants (60.7%) were in the pre-contemplative stage.
Conclusions
A high prevalence of hazardous drinking was recognized among online Vietnamese youths. In addition, we found relationships between alcohol use disorder and other addictive disorders, such as tobacco smoking and water-pipe usage. Our results highlighted that the majority of the individuals are not receptive to the idea of changing their alcohol habits, and this would imply that there ought to be more government effort towards the implementation of effective alcohol control policies.
I. Introduction
A recent report of the World Health Organization (WHO) highlights the global issue of alcohol use disorder [1]. It proposed that there needs to be further governmental efforts put in place to curb the increasing prevalence of this disorder [1]. According to the existing clinical guidelines, the intake of more than 40 g/day of alcohol for males and more than 24 g/day for females is considered to be hazardous alcohol consumption [2]. Prior studies have found an association between hazardous levels of drinking and the development of multiple medical comorbidities, such as hepatic dysfunction, seizures, neuropsychiatric conditions including anxiety and depression, as well as a heightened incidence of cancer, including that of the liver and breast [1].
The problem of alcohol use disorder is especially prevalent in Vietnam. Based on the latest WHO report [3], about 1.4% Vietnamese population were alcohol drinkers with the average alcohol consumption doubling from 3.8 liters in 2005 to 6.6 liters of alcohol in 2010 [3]. However, this statistic might be an underestimate because Vietnamese people in rural areas brew their own alcohol and statistics are lacking [4]. For example, in a nationally representative survey, 80% of male respondents reported drinking alcohol in the last 12 months, of which 40% were hazardous drinkers [5]. Hence, alcohol use disorder, along with its multiple medical and psychiatric comorbidities would eventually be a major public health epidemic and problem in Vietnam along with its rapidly progressing economy. However, there are no restrictions in the alcohol-related policies, and there are no health warning labels on alcohol advertisements and containers [3]. Additionally, there is no comprehensive governmental management plan or a taskforce to deal with this issue [3].
In addition to the growing incidence of alcohol consumption among the adult population, a growing concern also pertains to how the youth population might be affected. With rapid changes in the economy, Vietnam is now more commercialized and more connected to the rest of the world via the Internet and social media. Previous studies have reported that more than 60% of the Internet users in Vietnam are in the range of 15–34 years old [6]. The increased accessibility of the Internet might mean that more youths are exposed to social networking sites. One recent paper suggested that individuals, especially youths, who are exposed to social networking sites as well as smartphone applications are more easily influenced and tend to have a higher consumption of alcoholic beverages [7]. The impact of technological advances seemed to be most influential on youths. Other recent studies have reported that the absolute amount of time youths spent on social media networks correlated with the frequency of them having alcohol or even other addictive behaviors [8]. In addition, prior studies have also looked into youths' perceptions of alcohol-related advertisement on social media sites. Huang et al. [9] also highlighted how online interpersonal relationships might predispose individuals to using alcohol. Griffiths and Casswell [10] highlighted how the Internet allows youths to create “intoxigenic social identifies” and networks that have normalized their attitudes towards drinking. Thus, the introduction of technology has led to changes in perceptions of youths towards alcohol in developing countries.
Although the evidence of alcohol use among general Vietnamese population is available [5], there has been a lack of research on the rate of alcohol use in vulnerable groups, especially the youth population. Therefore, this study investigated the prevalence of alcohol use among Vietnamese youths in the Internet setting. In addition, it is also the objective of this paper to elucidate the associated factors that might predispose youths to alcohol-related disorders, such as high levels of perceived stressors in life, or having a poor health-related quality of life.
II. Methods
1. Study Design and Population
We conducted an online cross-sectional survey from August 2015 to October 2015 in Vietnam. Youths who met the following inclusion criteria as specified were invited to participate in the study: (1) belonging to the age group of 15 to 25 years, (2) living in Vietnam, and (3) having either an email account or an account on social networking sites to invite their peers. There were no specific exclusion criteria in this study.
2. Recruitment of Participants
In this study, web-based respondent-driven sampling (WebRDS) was used to recruit participants. We initially recruited core groups as ‘seeds’ regarding the differences of age group, sex, and education level, which could help to implement long recruitment chains to ensure that the sample would reach equilibrium [11]. We selected core groups from universities and high schools in Vietnam (Hanoi Medical University, Vietnam National University, Hung Yen High School, Phan Boi Chau High School). Based on the evaluation of student unions in each university/school, the core groups were chosen and contacted via phone and email if they were high-energy sociometrical stars and committed to being generative in recruiting their peers in the study. After completing the survey, the core groups were required to invite up to five peers via email or social media networks to participate in the online study. Those participants who had difficulties with accessing the original website (i.e., IP conflict, requested time out, etc.) were given another web-link with similar website content to facilitate their access. The recruitment chains were terminated when the recruitment network could not be expanded.
3. Sample Size
We used the formula of Wejnert et al. [12] for the RDS technique to calculate the sample size. With the expected prevalence of youths drinking alcohol in the last 30 days = 36.0% (according to a previous study in Vietnam [13]), confidence level = 95%, margin of error = 0.05, and design effect for RDS = 3, the minimum sample size was 1,065 youths. To prevent incomplete responses, 5% was added to the sample size. The final sample size was 1,118.
Core groups and piloted groups were included in the sample. Double participants were identified through duplication of email (n = 7). People who did not meet the eligible inclusion criteria were excluded (n = 3). We also excluded people who did not answer more than 60% of the questions in the study (n = 28). Finally, a total of 1,080 youths participated in the survey.
4. Conceptualization of Web Survey
Google Form, which met the privacy requirements of the ethical committee, was used to implement the online survey. A total of 40 questions were used in the survey, which required participants to answer within 15–20 minutes. Logic checks were performed to ensure that the participants answered correctly the theme of the questions. A pilot study with twenty youths was conducted to test the feasibility and reliability of the platform. During testing, the participants reported several issues regarding the accessibility of website, the content of the questionnaire, and the way to refer their peers. Because only minor changes occurred that did not influence the answers, the youths in the pilot study were included into the final sample.
5. Measurements
1) Alcohol use
To determine the absolute amount of alcohol usage and consumption, we used the Alcohol Use Disorders Identification Test-Consumption instrument (AUDIT-C), which is a shortened version of the Alcohol Use Disorders Identification Test (AUDIT). The Vietnamese version of this toolkit was utilized as it had been validated previously. The current tool consists of three questions about (1) frequency of drinking alcohol, (2) amount of drinks containing alcohol on a typical day, and (3) frequency of drinking six drinks or more on one occasion. The total score ranges from 0 to 12. The respondents were classified as hazardous drinkers if men had score ≥4 and women had score ≥3. Furthermore, the participants were also categorized as binge drinkers if the last item of the instrument received any positive response [14].
In addition, information about their motivation to quit alcohol consumption as well as the preferred methods to quit were also collated. To understand the motivation to quit alcohol drinking among respondents, we applied the transtheoretical model that describes the progressing of health behaviors through a series of five sequential stages of change. This includes (1) pre-contemplation, (2) contemplation, (3) preparation, (4) action, and (5) maintenance. A question was asked to the respondents: “Are you thinking about quitting alcohol use?” with five response levels—“No thought of quitting,” “Think I should quit but not quite ready”, “Start to think about how to change my alcohol drinking behavior,” “Take action to quit,” and “Already maintain quitting alcohol use” corresponding to the stages of (1) to (5). For alcohol drinkers who thought that they did not drink alcohol, we classified them into an ‘Others’ group. Participants were also asked to report their preferred method to quit, for example: support from health staff/relatives/friends, alcohol replacement therapies, medication, mobile phone application, etc. In addition, participant's willingness to pay for a smartphone application to help them in reducing and quitting alcohol was determined.
2) Covariates
(1) Baseline demographics
Socio-demographic information that was captured included age, gender, years of education, marital status, ethnicity, religious beliefs, as well as living location.
(2) Health status, health-related quality of life, and perceived stress
The health status of the participants was acquired by asking them whether they had suffered any acute diseases in the previous 4 weeks or chronic illness in the previous 3 months. We also identified whether participants were overweight/obese based on their self-reported height and weight. An individual was considered overweight/obese when he/she had body mass index more than 23 kg/m2.
Health-related quality of life (HRQOL) was measured by using the EuroQol-five dimensions-five levels (EQ-5D-5L) instrument. The descriptive system includes five domains: mobility, self-care, usual activities, pain/discomfort and anxiety/depression with five levels of response (no problems, slight problems, moderate problems, severe problems, and extreme problems), giving 3,125 health states with respective single indexes. To compute those indexes, the interim scoring for EQ-5D-5L from the cross-walk value set of Thailand was utilized due to the unavailability of Vietnamese population's preferences [15]. Additionally, the EQ-VAS was also used to assess the self-rated health of respondents on a 20-cm vertical scale, with the endpoint range from 0 to 100 point, labeled ‘the best health you can imagine’ and ‘the worst health you can imagine’. The Vietnamese version of EQ-5D-5L was translated and adopted as it had been previously validated [15].
The short-form Perceived Stress Scale (PSS) was used to measure perceived stress of participants in the previous 30 days. This instrument includes 4 items on a 5-point scale: never (0), almost never (1), sometimes (2), fairly often (3), and very often (4). There are two negative and two positive items. The total scores range from 0 to 16 for the 4-item scale. Higher scores indicate greater stress [16].
(3) Other risk behaviors
Participants were also asked about whether they had smoked cigarette and shisha (water-pipe) in the last month.
6. Statistical analysis
Chi-squared and t-test analyses were used to explore the differences among the variables. Multivariate logistic regression was utilized to identify the associated factors. In this study, we applied a stepwise forward model strategy using a log-likelihood ratio test at a p-value of 0.2 to select variables for the reduced models [17]. A p-value of less than 0.05 was set as the level of statistical significance.
7. Ethical Approval
The proposal of this study was approved by the Vietnam Authority of HIV/AIDS Control of the Vietnam Ministry of Health. All participants were required to provide electronic information consent and they were advised that they could withdraw anytime. Their responses were coded and they were assured that the information that they provided was confidential.
III. Results
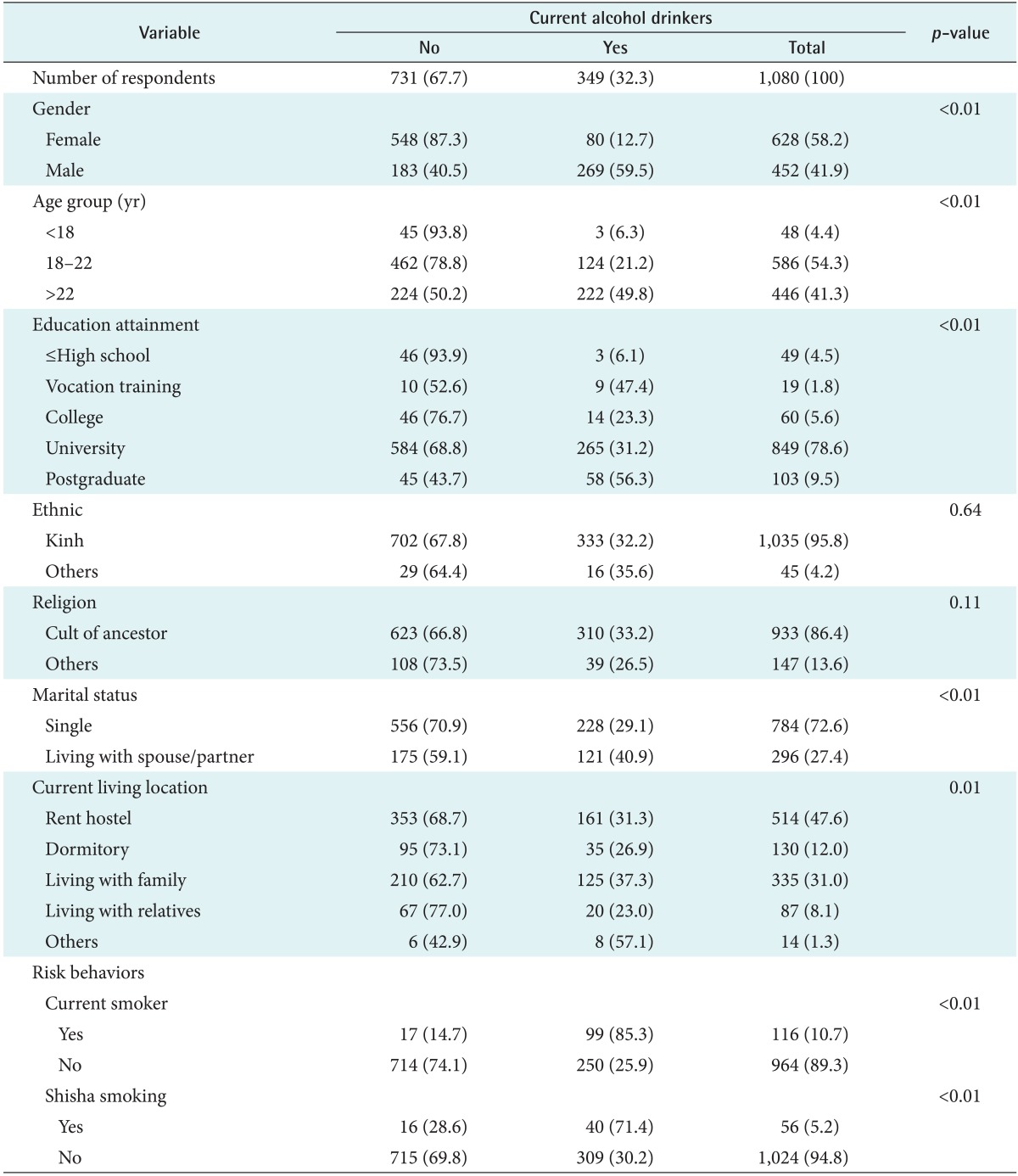
Table 1 presents the demographic characteristics of the participants. A cumulative total of 1,080 youths were recruited via the sampling methodology. Of the youths recruited 52.8% were female, and the remaining 41.9% were male. In all, 59.5% males and 12.7% of youths declared that they were actively using alcohol. The vast majority of the participants were between 18 and 22 years of age, accounting for 54.3% of the total sample. Most of the participants (78.6%) had obtained university education. The majority of the participants were of Kinh ethnicity (95.8%), and most were single (72.6%) and were staying in a hostel (47.6%) when they were recruited. Of significance, a cumulative total of 10.7% of the participants were current smokers, and another 5.2% of the participants were water-pipe (Shisha) smokers.
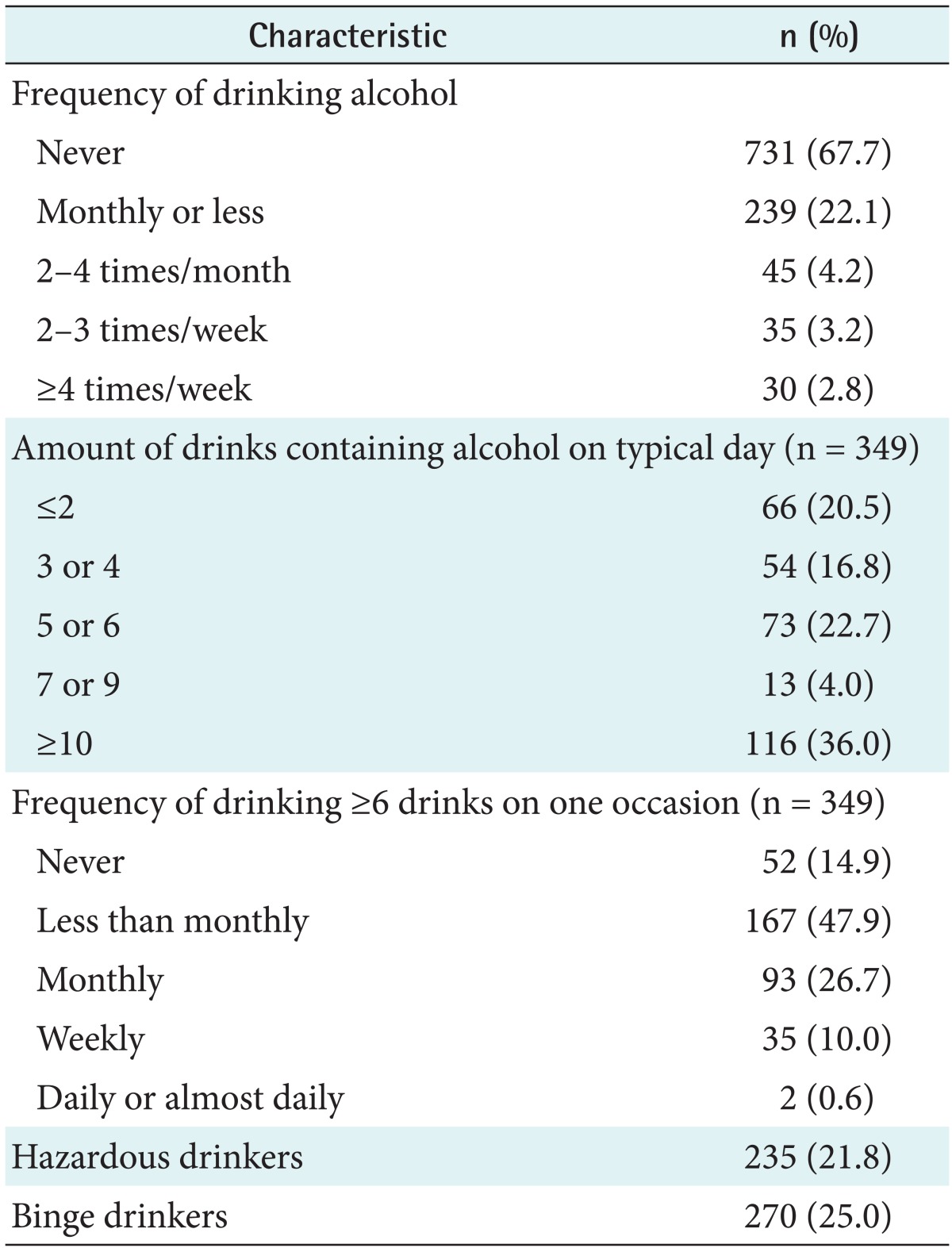
Table 2 shows that a cumulative total of 32.3% of the participants were drinking alcohol, with 21.8% and 25.0% of the participants being classified as drinking hazardously and binge drinkers, respectively.
Table 3 presents the general health status of the respondents. About 17.5% of active drinkers were overweight as compared to 5.3% of those who were not drinking. There were no significant differences in the various domains of the HRQOL for most of the participants who were drinking and not drinking alcohol, with the exception that those who were actively drinking had more significant problems with their self-care. Of note, there were no statistically significant differences in the EQ-5D index, EQ-VAS, and PSS.
Table 4 presents the alcohol drinking quitting pattern among the participants. The majority of the participants (60.7%) were pre-contemplative, in that they did not feel that they had an alcohol issue. Only 11.6% had contemplated their problem, and only 2.9% and 6.7% were in the preparation and action phases with regards to changing their alcohol habits. For those who were using alcohol, the preferred methodology for them to quit alcohol usage was to use a replacement liquid (8.9%). The majority also perceived that support from relatives and friends was important and helpful. Notification from mobile phone was not perceived to be very useful for this group of participants. Out of the entire sample, only 19.2% of the participants indicated that they were willing to pay a median of VND 50,000 (USD 2.24) for a smartphone application to help them.
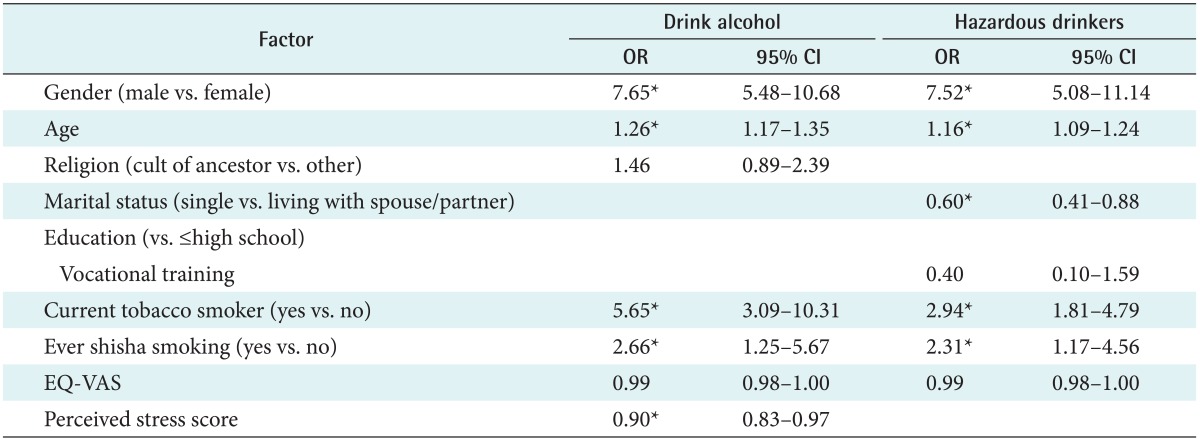
Table 5 presents an analysis of the factors that are associated with individuals who are drinkers or drinking hazardously. Of significance, drinking alcohol was positively associated with males (odds ratio [OR] = 7.65; 95% confidence interval [CI], 5.48–10.68) and higher age (OR = 1.26; 95% CI, 1.17–1.35). Individuals who were current smokers were 5.65 times more likely to drink alcohol (OR = 5.65; 95% CI, 3.09–10.31) than non-smokers. Meanwhile, higher perceived stress score was negatively related with higher likelihood of being an alcohol drinker (OR = 0.90; 95% CI, 0.83–0.97).
Regarding hazardous drinkers, people who were male (OR = 7.52; 95% CI, 5.08–11.14), older (OR = 1.16; 95% CI, 1.09–1.24), current smokers (OR = 2.94; 95% CI, 1.81–4.79) and had ever smoked shisha (OR = 2.31; 95% CI, 1.17–4.56) were more likely to be hazardous drinkers. Meanwhile, people who were single were less likely to drink hazardously compared to those living with a spouse/partner (OR = 0.60; 95% CI, 0.41–0.88).
IV. Discussion
While there have been prior studies looking into alcohol and its associated harmful effects among the youth population in the Internet setting in Vietnam [18], this is one of the first studies to utilize e-health to determine the severity of alcohol use disorders among an Internet sample of youths and to determine associated factors that might predispose these individuals towards alcohol usage. Surveying an Internet cohort of participants would share insights into how the introduction of e-health technologies in a developing country might affect the severity of alcohol use disorders. The obtained results demonstrate that our sampled population has a relatively high level of educational attainment, with the vast majority having at least a university education. Of importance, approximately 5.2% and 10.7% of the sampled population were already using other substances, such as tobacco and water-pipe (shisha). The results also demonstrate that an alarming 21.8% and 25% of the sampled individuals were using alcohol hazardously, or were binging on alcohol as well. Those who were drinking alcohol hazardously were noted to be overweight, which might be due to the adverse caloric effects of chronic alcohol use. Of note, the majority of those sampled were ambivalent and pre-contemplative about cutting down their alcohol use. A further statistical analysis also revealed that there is a correlation between alcohol usage and other risky behaviors, such as tobacco and waterpipe usage.
Notably, our prevalence result is similar to the result of a national survey on adolescents and youths in Vietnam, which used a face-to-face approach and found that 36% of participants aged from 14–25 years had drank alcohol in the last 30 days [13]. Another study among Vietnamese medical students using the paper-pencil method showed that 57.5% of participants had drank alcohol in the previous 12 months [18]. The differences might be explained by the differences in the sample and the measurement of each study. A previous study suggested that Internet-based survey has the advantages of the anonymity of participants and convenience for researchers in storing data in electronic databases [19]. Further studies are warranted to compare the usability of Internet-based surveying and other survey methods in examining alcohol use behaviors.
Our results are consistent with those of a previous study by Kaljee et al. [20]. Their findings showed that approximately 29.2% of their sampled population had had alcohol use disorder, and females were more likely to have indulged in binge drinking and were more likely to have suffered from intoxication within a 6-month period [20]. Their initial study already highlighted that, since 2005, there has been an increasing trend of youths consuming alcohol at a younger age. At the same time, there is perhaps a multitude of factors that might predispose youths in Vietnam towards increased consumption of alcohol. One of the main factors might be the changes in the economy in Vietnam, with more commercialization and globalization taking place. In addition to the changes in the economy, there are other factors, such as attainment of better and higher education as well as an increase in technological access. Previous studies have examined the impact of social media on alcohol consumption in adolescents and young adults [21]. These studies have highlighted the close relationship and association between the exposure youths and young adults get from social networking and Internet sites and the amount of alcohol they eventually consume [21]. Health behavior theories, such as the social learning theory, could potentially account for the changes in youths and young adult's behavior. More recent studies have highlighted that besides conventional methodologies of marketing and promoting alcohol consumption, the Internet, and various digital media and social network sites are increasingly being used to promote the use of alcohol [7]. Although we have not managed to elucidate the extent to which youths and adolescents in our sample used the Internet and social networking sites, it is inevitable that along with the introduction of the Internet in Vietnam, youths and adolescents are at risk of greater exposure. Another issue pertains to the alcohol control policies that are currently in place in Vietnam. Prior research has demonstrated that the amount that youths and young adults are drinking is highly dependent on environmental factors [22], in particular, the availability of alcohol and the density of drinking places [22]. Alcohol control policies have been shown to be effective in controlling the prevalence of alcohol-use disorders [23]. Vietnam, to our knowledge, does not have a concrete alcohol control policy that is comparable to other countries, such as restrictions on the timing of alcohol sale and the sites at which alcohol can be consumed.
Our current research highlighted that there are no significant differences in the various domains of physical health among those who use alcohol as compared to those who do not use alcohol, with the exception that those who use alcohol hazardously tend to be overweight. Excessive alcoholic consumption and its detrimental impact on college students have previously been extensively studied [24]. While prior research suggested that the most common consequences are overdoses and memory blackouts, it is expected that there might be metabolic and physical changes over time for those who consume alcohol hazardously. This is in view of the fact that an average drink would provide a significant amount of calories [25]. Lastly, our results also highlighted an association between the use of tobacco and shisha and alcohol use disorder. Our findings agree with prior research findings, which suggest that there are significant correlations between water-pipe smoking, drug usage, and alcohol and tobacco usage [26]. Other risky behaviors, such as water-pipe smoking as well as tobacco use, might be gateways towards predisposing youths to alcohol use and dependence.
Our findings also demonstrate that the majority of our online sample of youths are in the pre-contemplative and contemplative stages of change, and these findings agree with those of prior studies [27]. One of the key findings in our study pertains to how participants perceive the effectiveness of having a smartphone-based application to help them with their alcohol use disorder. The vast majority of the participants felt that notification was a useful reminder, which agrees with our previous study of a new alcohol tracker application amongst a Canadian cohort of university students [28]. Various other studies have demonstrated how mobile phones are useful in helping reduce unhealthy use of alcohol and facilitate the delivery of psychological interventions, such as commitment and acceptance therapy in motivating change [2930]. There remains a lack of examination of the existing applications in Vietnamese application stores, and future research ought to examine their evidence base so that there could be a repository of applications that could be recommended by clinicians to individuals.
The strength of our current research is that we managed to recruit a large sample of participants and therefore managed to determine the severity of alcohol use disorder amongst the sample recruited. Our current study also demonstrated the utility of e-health and its potential in the assessment of individuals for various disorders, as established by prior research. The significant advantage of using technology in assessing the severity of a particular condition in the general population is that it is much faster in the acquisition of data than conventional sampling mechanisms, and it is relatively more cost-effective as well.
There were several limitations in our current study. Although we managed to recruit a substantial number of individuals to determine the overall prevalence of hazardous drinking, the prevalence data could have limited generalization to the entire Vietnamese population, given that individuals in rural areas of Vietnam were not included. In addition, as the mechanism of recruitment was via the Internet, we were not able to measure the amount of alcohol-use disorders among individuals of similar ages who did not have access to the Internet. While we have shown that access to the Internet might have changed individuals' perceptions and caused them to drink more, we have not, in our questionnaire, asked specifically about their degree and amount of Internet usage.
In conclusion, this is perhaps one of the first studies to make use of e-health to determine the severity of alcohol use disorder amongst an online sample of participants as well as the factors that might predispose individuals to use alcohol. Our findings may be instrumental in providing guidance to existing governmental policies as well as guiding future ehealth interventions in this area in Vietnam.
Acknowledgments
The authors would like to acknowledge supports by the Vietnam Authority of HIV/AIDS Control for the implementation of the study.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.