I. Introduction
The benefits of physical exercise for breast cancer (BC) patients and survivors are widely recognized. A recent meta-analysis revealed that physical activity (PA) can reduce both BC mortality and overall mortality rates. Notably, women with BC who engage in high levels of recreational activities have a lower risk of all-cause mortality and BC-related death than those who participate in lower levels of activity [
1]. Consistent participation in PA can help to maintain and enhance cardiopulmonary function, muscle strength, and cancer-related fatigue. It can also improve quality of life (QoL) and other aspects of psychological health in cancer survivors [
2,
3].
Since the advent of telemedicine in the 2000s, the wide-spread use of the internet and smartphones has spurred the rapid expansion of mobile health [
4]. The recent coronavirus disease 2019 pandemic has further heightened the demand for digital health technologies.
Digital health interventions (DHIs) are defined as the use of technologies, including text messaging, emails, mobile applications, videoconferencing, social media, websites, and online portals, for the purpose of promoting health promotion or treatment adherence [
5]. The impact of DHIs has been widely investigated due to their immense potential in areas such as efficacy, cost-effectiveness, safety, and scalability [
6]. DHIs have been implemented to boost medication adherence, foster smoking cessation, and encourage PA [
7,
8]. They also aim to improve health outcomes for long-term conditions and offer remote access to treatment for individuals grappling with mental health and somatic issues [
9,
10].
Although studies have explored the effects of DHIs, the findings regarding their effect on increasing PA are often inconsistent. Roberts et al. [
5] found that DHIs targeting PA and diet significantly increased moderate and vigorous PA per week and reduced body mass index (BMI) among cancer survivors, irrespective of the type of cancer. More recently, Singleton et al. [
11] carried out a systematic review and meta-analysis on health interventions using electronic technologies for BC patients. However, only three studies focusing on PA-related patient-reported outcomes were included in the review. It has been reported that these individuals are at risk of maintaining sedentary behaviors following a BC diagnosis and often do not adhere to the appropriate PA level recommended by expert-developed health behavior guidelines [
12]. Despite this, research findings suggest that PA is beneficial for BC patients undergoing active treatments and for survivors who have completed treatments [
2,
3]. Given the importance of improving PA to maximize treatment effects and various aspects of positive health outcomes, it is crucial to gain a clear understanding of the impact of digital PA interventions. Therefore, this study conducted a systematic review and meta-analysis to evaluate the effects of digital PA interventions provided for BC patients and survivors on improving PA and QoL.
III. Results
1. Search Results
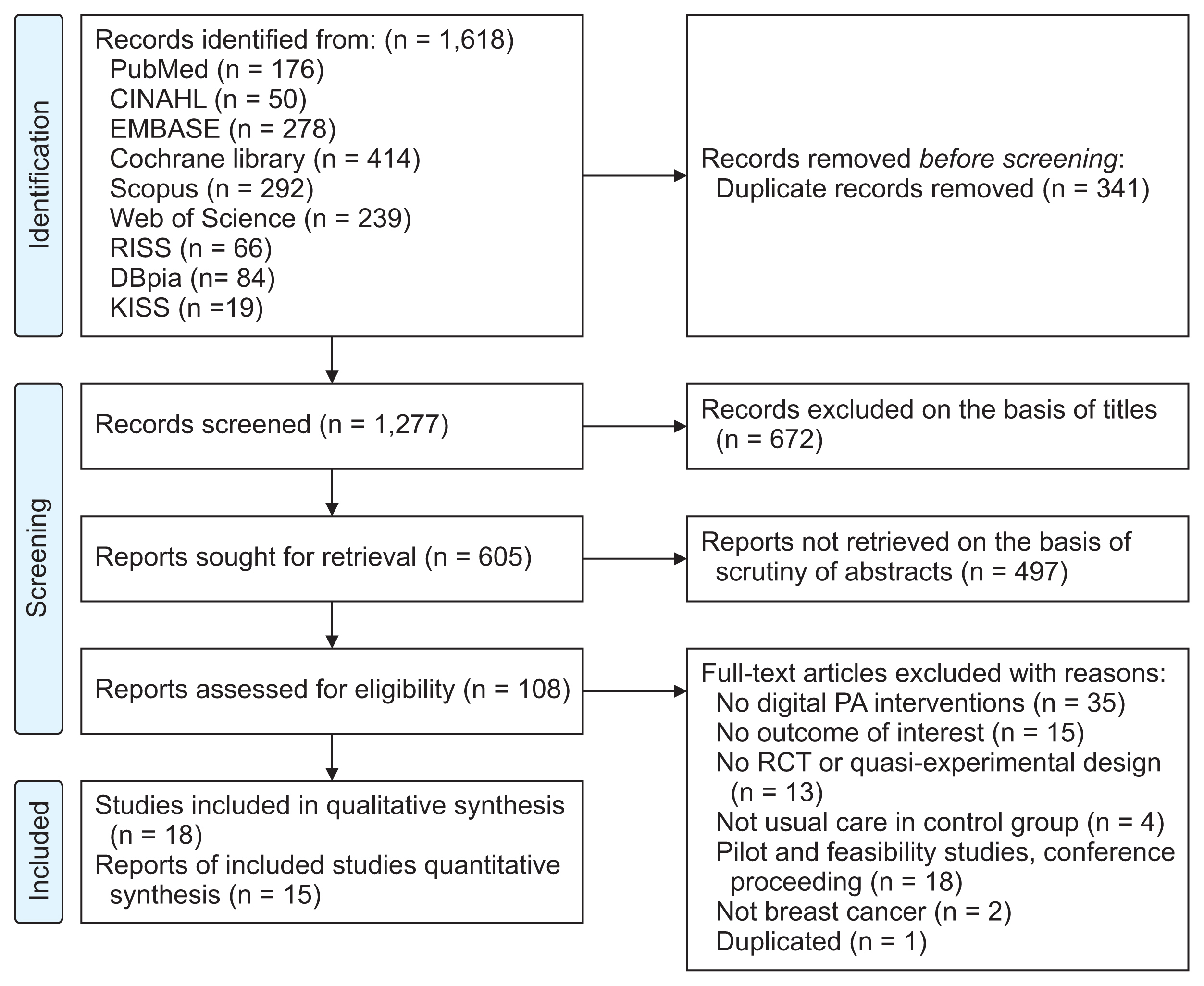
As depicted in
Figure 1, the initial search of eight databases yielded 1,618 records. Once 341 duplicates were eliminated, 1,277 titles remained for review, leaving 605 records for abstract review. Following the exclusion of 497 records post-abstract review, 108 full-text articles were obtained. Out of these, 90 records were excluded as they failed to meet the inclusion and exclusion criteria, leaving 18 studies for consideration. Three studies (A3
a,b, A7
a,b, A15
a,b) were published in two or more journals with different variables, and we only included journal articles published with PA- or QoL-associated outcomes.
2. Characteristics of the Included Studies
Among the 18 selected studies, 16 were RCTs and two were quasi-experimental studies (
Table 1). All studies were conducted after 2010. Specifically, 10 studies took place between approximately 2013 and 2019, while the remaining eight studies were conducted from 2020 to 2022. In terms of geographical distribution, three studies were conducted in the United States, three in South Korea, and two each in Australia, Spain, and Turkey, with the remaining studies taking place in Canada, China, Germany, Japan, and Taiwan. The total number of participants across all studies was 1,703. The duration of the interventions ranged from 3 weeks to 12 months. However, the majority of the studies (72%, n = 13) had an intervention period of 12 weeks.
Approximately 50ŌĆō100 participants were involved in 12 of the studies, while four studies had more than 100 participants, and two studies had fewer than 50 participants. The average age of the participants ranged from 41.5 to 62 years. In terms of BC stages, 12 studies included participants in stages 0ŌĆōIII or those without metastasis, two studies included participants with metastasis (A4, A16), and four studies did not consider the cancer stage as a criterion for inclusion (A1, A9, A14, A17). Studies that included only participants with metastasis aimed to improve QoL (A4, A16) or reduce the side effects of chemotherapy (A4) by promoting PA, rather than increasing the duration of PA or functional capacity. All participants were women, but only 50% (n = 9) of the studies specified female sex as an inclusion criterion. Additionally, some studies included criteria such as limited moderate-to-vigorous physical activity (MVPA) (A2, A7b, A8, A10, A16, A18) or a BMI of Ōēź23 kg/m2 (A10, A12, A15).
3. Quantitative Analysis of PA Outcomes
1) PA duration
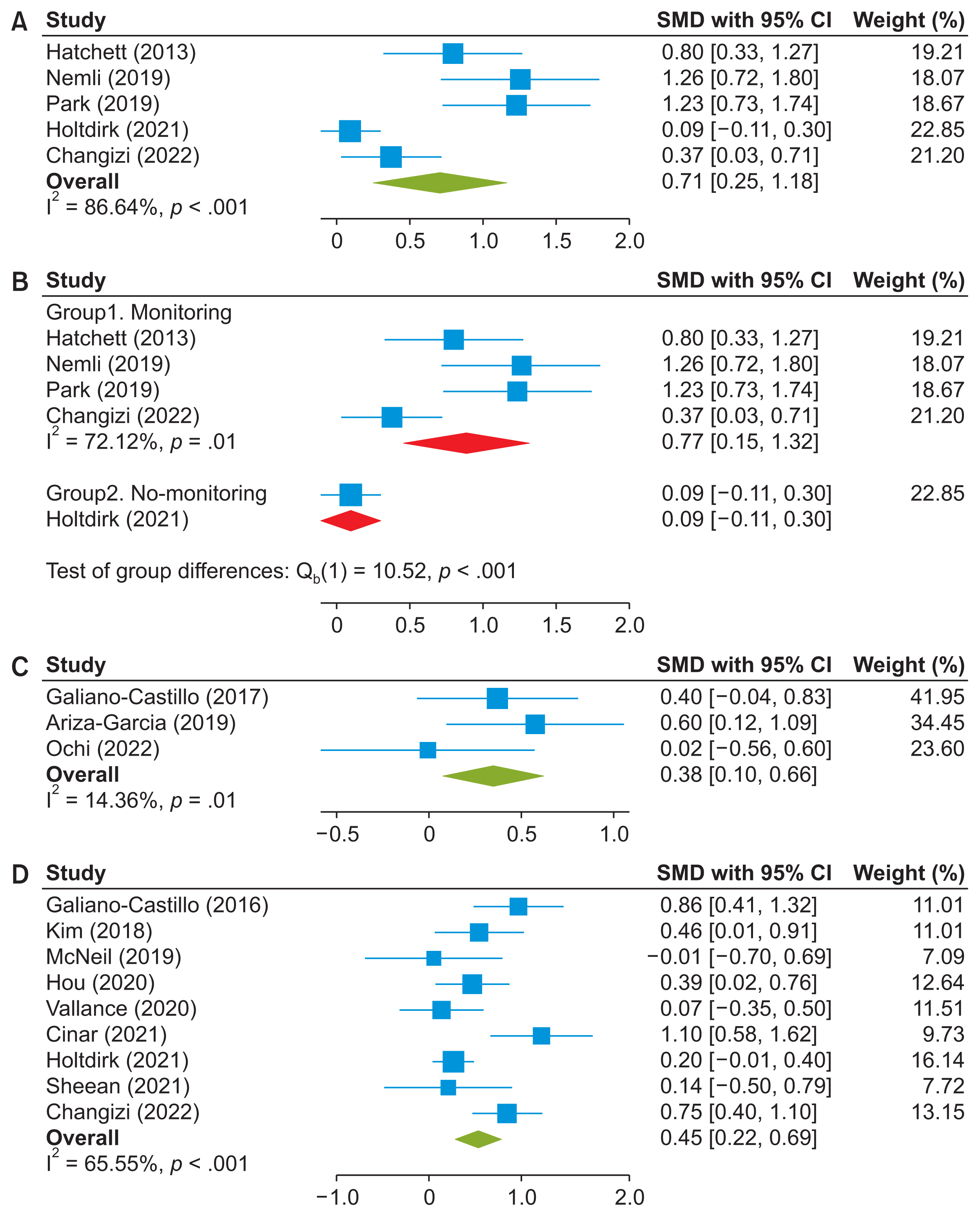
Five studies (A1, A9, A10, A14, A17) reported pre- and post-treatment PA duration using IPAQ and the PAR data, which could be combined for meta-analysis; these studies included 41% of participants in the systematic review. Follow-up data were excluded from the analysis due to the significant variation in follow-up periods across the studies. The total PA time from each study was aggregated using a random effects model with HedgesŌĆÖ g. The meta-analysis results comparing the intervention and control groups are illustrated in
Figure 2A. The overall effect size was 0.71 (95% [CI], 0.25ŌĆō1.18), indicating a significant improvement in PA duration with substantial heterogeneity (I
2 = 86.64%).
The results for the subgroup analysis according to whether there was feedback or monitoring for participantsŌĆÖ performance (monitoring vs. no-monitoring) are presented in
Figure 2B. The monitoring group showed a significant improvement in PA duration (SMD = 0.88; 95% CI, 0.45ŌĆō1.32; I
2 = 72.12%), whereas the effects of the interventions without monitoring were not statistically significant.
2) Physical function
Three (A3
b, A5, A18) of 18 studies (6% of participants) evaluated functional capacity using the 6MWT. These three studies were pooled in a fixed-effect meta-analysis. A significant improvement was observed in the intervention group compared with the control group (SMD = 0.38; 95% CI, 0.10ŌĆō0.66; I
2 = 14.36%) (
Figure 2C).
3) Quality of life
Nine studies (A3
a, A4, A7
b, A8, A11, A13, A14, A16, A17) were included in the meta-analysis of QoL. Using data from 57.4% of the total participants, there was a significant pooled improvement in QoL (SMD = 0.45, 95% CI, 0.22ŌĆō0.69; I
2 = 65.55%) (
Figure 2D).
4. Qualitative Analysis of PA and QoL Outcomes
1) PA-related outcomes
The outcome measures related to PA in digital PA interventions included the duration of PA in daily life and the level of functional capacity. Seven studies (39%) utilized instruments or questionnaires to measure self-reported PA duration. These included the PA recall (A1), the IPAQ (A9, A10, A14, A17), global PA questionnaires (A18), or the weekly duration of MVPA (A2). Only two studies (A8, A15a,b) employed wearable devices, such as an actigraph, to objectively measure the duration of PA. Most studies reported that the intervention groups significantly increased their PA duration compared to the control groups. However, two studies (A14, A15a,b) did not observe any significant differences between the groups.
In addition to PA duration, functional capacity was evaluated by measuring the 6MWT, 2MWT, and muscle strength of the abdomen, upper, or lower limbs, or grip strength (A3a,b, A5, A6, A18). Significant between-group effects were noted in some or all variables. Four studies (A5, A8, A10, A12) evaluated anthropometrics, including BMI and waist and hip circumferences, and the intervention effects were inconsistent between studies.
2) QoL outcomes
QoL was measured in 14 studies, of which 11 observed significant intervention effects (A2ŌĆōA4, A6, A9, A11, A13ŌĆō17). Of these studies, 64.3% (n = 9/14) used cancer- or BC-specific measurements, including the EORTC QLQ-C30 [
17] (A2, A3
a, A11, A17), EORTC QLQ-BR23 [
18] (A9, A11), FACT-B [
19] (A7
b, A8, A16), and FACT-ES [
20] (A13). The other studies used global QoL or health-related QoL measures, including WHO QoL-BREF [
21] (A4, A14), SF-12 [
22] (A8), SF-36 [
22] (A6), PROMIS Global Health Scale [
23] (A15
a), and EQ-5D (A18). One study (A8) used both BC-specific and global QoL measurements.
5. Components of Digital PA Interventions
As shown in
Table 2, a substantial majority of the studies (83.3%) employed multi-component interventions. These primarily included (1) training or encouraging PA, (2) monitoring participantsŌĆÖ performance either by the research team or through self-monitoring, and (3) offering feedback or peer support. The application of digital technologies varied in the delivery of these interventions.
- Mobile applications: Half of the studies (A4, A6, A8, A10ŌĆōA13, A17, A18) utilized mobile applications or games to deliver disease-related education (A4, A6, A11ŌĆōA13), PA training (A13, A17, A18), monitor PA participation (A8), and provide peer support (A10). The intervention group demonstrated a significant increase in PA in all studies, with the exception of the study by Ochi et al. (A18).
- Websites or internet modules: Three studies (A2, A3a,b, A5) employed websites to offer individualized exercise programs and monitor PA participation (A12). Additionally, one study (A14) utilized Internet modules to provide information on health behaviors, including PA.
- Emails: Two studies (A1, A18) used email messages as a means to encourage PA.
- Telephone or text messages: Telephone calls or text messages were used in studies A7, A9, and A13 to provide counseling or follow-up on PA participation, and in studies A15 and A16 for PA training.
- Wearable devices: Five studies (A7a,b, A8, A15a,b, A16, A18) incorporated wearable devices, such as activity trackers or pedometers, into their interventions to monitor participantsŌĆÖ PA levels.
All studies except for three studies (A4, A11, A14) implemented interventions using a combination of two or more technologies.
6. Retention and Sustainability and Theories for Intervention Development
The overall retention rates were high, ranging from 67.7% to 100%. No serious intervention-related adverse events were reported. Four studies (A3a,b, A8, A14, A15a,b) measured the sustained between-group effects of digital PA interventions at 24 weeks (A8), 6 months (A3a,b, A14), and 18 months (A15a,b). The intervention effects were maintained in three studies (A3a,b, A14, A15a,b); however, in one study (A8), the intervention effects declined and became non-significant between the groups. Attrition was minimal at follow-up in three studies (A3a,b, A8, A15a,b); however, one study (A14) reported that the attrition rates increased from 15.7% to 25.7% at the 6-month follow-up.
Six studies applied theories associated with health behavior promotion, including the social cognitive theory (A1, A10, A15
a,b, A16, A18) and the transtheoretical model [
24] (A2). Three (A1, A2, A10) studies explicitly described theoretical underpinnings and how the theory was used to develop the interventions and measured the main constructs such as self-efficacy (A1, A2, A10), stage of change (A2), or motivation (A10). Two studies (A1, A2) significantly increased the self-efficacy for exercise, and Lee et al. (A2) reported a significant increase in the stage of change in the intervention groups. The other studies (A15
a,b, A16, A18) provided a brief explanation about the major concepts of theories; their interventions were grounded and did not measure the theoretical construct.
7. RoB Assessment
Among 16 RCTs, 2 (A7
a,b, A17) had concerns in the randomization domain since they did not clearly describe the randomization process and allocation concealment (
Figure 3). Owing to the nature of the studies, no studies blinded the participants and only some blinded the assessors. This fact increased the risk of bias in the measurement of the outcome domain since 44% of studies (A8, A9, A12ŌĆōA17) used self-report outcome measures, for which the assessment of the outcome could be potentially skewed based on the participantsŌĆÖ knowledge of their group assignment status.
8. Publication Bias
The results of the Egger regression test to assess the publication bias for studies with functional capacity (
p = 0.28) and QoL (
p = 0.93) showed no evidence of publication bias. However, publication bias for the studies with total PA times was observed (
p < 0.001) and corrected using the trim-and-fill method [
25].
IV. Discussion
The findings of this study showed that digital PA interventions significantly improved the PA and functional capacity of BC patients and survivors. The meta-analysis of pooled data from fivve studies (A1, A9, A10, A14, A17) showed that digital PA interventions significantly increased PA duration with a medium effect size (SMD = 0.71; 95% CI, 0.25ŌĆō1.18) and high heterogeneity (I
2 = 86.64%). The qualitative analysis of the other included studies also showed significant intervention effects, demonstrating that digital PA interventions are promising interventions that actually improve exercise participation among patients with BC. The result regarding PA duration agrees with a previous study conducted by Roberts et al. [
5] who reported that DHIs for cancer survivors significantly increased MVPA, with considerable heterogeneity (effect size = 41.5, I
2 = 81.3%).
Among the five studies included in the meta-analysis of PA duration, only the study by Holtdirk et al. (A14) observed no significant between-group effects. This studyŌĆÖs intervention components differed from the other three studies that did demonstrate significant between-group effects. The intervention in this study did not involve any interaction or feedback with providers during the study period. In contrast, the other three studies included regular interactions with the research team via text messages (A17), phone calls (A8), or self-monitoring (A9) as key elements of their interventions. However, another study (A15a,b), not included in the meta-analysis, involved consistent interaction with participants through phone calls and optional texts. Despite a relatively long intervention period (12 months), this study reported non-significant findings for PA-related outcomes. Therefore, additional research is required to determine which component would effectively contribute to improving PA in this population.
Various combinations of digital technologies, including mobile applications, telephone, text messages, and websites, have been used to deliver digital interventions. Furthermore, these digital technologies were applied to different roles, such as PA training or encouragement (A1, A2, A3a,b, A5, A13, A15a,b, A16, A17, A18), disease- or treatment-related education (A4, A6, A11ŌĆōA13), monitoring PA performance (A7a,b, A8, A12, A15a,b, A16, A18), and/or feedback or peer support (A7, A9, A10, A13). The specific subtypes or dosage of interventions did not seem to significantly impact the improvement of PA duration. For instance, the use of a single mode such as email messages (A1), as well as the combined use of multiple technologies like mobile applications, telephone calls, and/or text messages (A8, A12, A13), led to a significant increase in PA, despite the relatively small sample size. However, determining the most effective combination of digital technologies to enhance PA in this population proved challenging. Further research is required to compare the effects of PA interventions that utilize different technologies.
A meta-analysis of the 6MWT with three studies (A3
b, A5, A18) showed that digital PA interventions effectively increased functional capacity with a medium effect size (SMD = 0.38; 95% CI, 0.10ŌĆō0.66; I
2 = 14.36%). This finding is supported by previous studies reporting that exercise training improved exercise capacity and endothelial function [
26]. Functional capacity is linked to the ability to carry out activities primarily under aerobic conditions, which involves the integration of the cardiovascular, pulmonary, and skeletal muscle systems [
27,
28]. Consequently, the improvement in PA observed after participating in interventions could lead to an increase in functional capacity.
A meta-analysis of QoL using pooled data from nine studies showed a significant intervention effect (SMD = 0.45; 95% CI, 0.22ŌĆō0.69; I
2 = 65.55%). This finding suggests that digital interventions promoting PA effectively improved the QoL of BC survivors and patients. Conversely, a prior meta-analysis conducted by Roberts et al. [
5] did not identify a significant improvement in cancer-specific QoL following the implementation of DHIs for cancer survivors. However, a direct comparison is not feasible since the study by Roberts et al. [
5] only incorporated five studies in their review, which included both RCTs and pre-post designs, and did not limit the types of cancer.
The overall retention rate of the included studies was high; however, there was insufficient evidence regarding sustainability. Only four studies (A3
a,b, A8, A14, A15
a,b) examined sustained effects post-intervention, with three of these studies reporting that the intervention effects were maintained. Kabore et al. [
29] identified several barriers to the sustained effects of DHIs, including user integration with the technology, lack of staff and expertise, and barriers related to age, language, myths, and misconceptions. Given the rapid advancement of digital health technology and the high prevalence of BC, there is an urgent need to examine the long-term effects of digital PA interventions for this demographic.
This study had some limitations. First, the majority of participants in the chosen studies were in their 40s or 50s. Given the rising prevalence of BC in older age groups, the findings of this study may not be broadly applicable to older individuals with BC. Second, the RoB assessment results suggest that evaluating the effects of interventions could be challenging, primarily due to the reliance on patient-reported outcome measurements for PA. Given the nature of the studies, where blinding participants was not feasible, the subjectivity of these measurements could impede an accurate estimation of PA changes, thereby complicating the interpretation of the impact of digital PA interventions. Lastly, the meta-analysis of the pooled effect of PA duration demonstrated a high degree of heterogeneity stemming from variations in the intervention, the intervention group, or the data analysis method [
30]. A high level of heterogeneity is problematic as it can render the efficacy of interventions unpredictable when applied to new participants [
30]. Conducting RCTs to investigate the effects of interventions with similar delivery modes and employing objective measures could aid in comparing and identifying the most effective PA-promoting intervention. Despite these limitations, this study holds significance as it offers the most recent evidence and current understanding of the effects of digital PA interventions, by selecting relatively high-quality studies for BC patients and survivors.
In conclusion, this systematic review and meta-analysis demonstrated that digital PA interventions for BC patients and survivors effectively increased daily PA duration, functional capacity, QoL compared to usual care. A variety of digital technologies were employed to deliver PA training, disease-related education, and feedback or reminders from a third party or for self-monitoring, all of which effectively increased PA. Moreover, the high overall retention and compliance rates suggest that this population may encounter minimal barriers when participating in digital PA interventions. Further research is needed to explore the long-term effects of digital PA interventions and to conduct studies with older BC patients and survivors.